What are the symptoms of ventricular fibrillation?
Ventricular fibrillation (VF) is a serious and life-threatening arrhythmia where the heart’s ventricles quiver ineffectively instead of contracting properly, leading to a lack of blood flow to the body. Symptoms of ventricular fibrillation include:
1. Sudden Collapse:
- Loss of Consciousness: Patients often collapse abruptly and become unconscious due to the heart’s inability to pump blood effectively.
2. Sudden Cardiac Arrest:
- No Pulse: The heart stops beating effectively, leading to a cessation of blood flow, which is a hallmark of cardiac arrest.
3. Chest Pain:
- Severe Pain: Intense chest pain or discomfort can precede VF, but in many cases, symptoms may not be evident until collapse occurs.
4. Shortness of Breath:
- Breathlessness: Severe difficulty breathing may occur, but it often accompanies other symptoms or happens suddenly.
5. Dizziness or Lightheadedness:
- Fainting: A feeling of dizziness or lightheadedness, often leading to loss of consciousness.
6. Palpitations:
- Irregular Heartbeats: The sensation of rapid, irregular, or fluttering heartbeats may be felt before the onset of VF.
7. Cyanosis:
- Bluish Skin: A bluish discoloration of the skin or lips due to lack of oxygenated blood.
8. Seizures:
- Uncontrolled Movements: In some cases, seizures may occur due to the lack of oxygen to the brain.
9. Dilated Pupils:
- Pupil Changes: Pupils may become dilated and unresponsive to light.
Ventricular fibrillation is a medical emergency that requires immediate treatment. If you suspect someone is experiencing VF or sudden cardiac arrest, it’s critical to call emergency services and initiate cardiopulmonary resuscitation (CPR) while awaiting professional help. Early defibrillation using an automated external defibrillator (AED) can be crucial in restoring a normal heart rhythm.
What are the causes of ventricular fibrillation?
Ventricular fibrillation (VF) can be caused by various factors that disrupt the heart’s electrical system and lead to chaotic, ineffective heartbeats. Common causes include:
1. Coronary Artery Disease:
- Heart Attack: Blockages in the coronary arteries can lead to myocardial infarction (heart attack), which may trigger VF.
- Ischemia: Reduced blood flow to the heart muscle can cause electrical instability and lead to VF.
2. Cardiomyopathy:
- Dilated Cardiomyopathy: Enlargement and weakening of the heart muscle can disrupt normal electrical conduction.
- Hypertrophic Cardiomyopathy: Thickening of the heart muscle can alter electrical pathways and trigger VF.
3. Electrolyte Imbalances:
- Abnormal Levels: Imbalances in potassium, calcium, or magnesium can affect the heart’s electrical stability and lead to VF.
4. Heart Failure:
- Chronic Heart Failure: Advanced heart failure can cause electrical disturbances and increase the risk of VF.
5. Arrhythmias:
- Previous Arrhythmias: Conditions such as atrial fibrillation or other arrhythmias may precede VF.
6. Structural Heart Abnormalities:
- Valvular Heart Disease: Problems with heart valves can lead to electrical instability and contribute to VF.
- Congenital Heart Defects: Certain birth defects can predispose individuals to VF.
7. Myocarditis:
- Inflammation of the Heart Muscle: Inflammation due to infections or autoimmune conditions can disrupt the heart’s electrical system.
8. Drug Toxicity:
- Medications or Recreational Drugs: Some drugs, including stimulants and certain antiarrhythmics, can increase the risk of VF.
9. Genetic Factors:
- Inherited Conditions: Genetic disorders such as Long QT Syndrome or Brugada Syndrome can predispose individuals to VF.
10. Trauma:
- Physical Injury: Severe chest trauma or electrical shock can lead to VF.
11. Hypoxia:
- Oxygen Deprivation: Severe lack of oxygen to the heart or body can trigger VF.
12. Severe Bradycardia:
- Slow Heart Rate: Extremely slow heart rates can sometimes degenerate into VF.
13. Cardiac Surgery:
- Post-Surgical Complications: Surgery or interventions that affect the heart’s electrical system can sometimes lead to VF.
Addressing the underlying cause of VF is crucial in treatment and prevention. Immediate medical attention is required for VF to restore a normal heart rhythm and manage any contributing factors.
What is the treatment for ventricular fibrillation?
The treatment for ventricular fibrillation (VF) focuses on restoring a normal heart rhythm and ensuring that blood flow is reestablished. Immediate and effective intervention is crucial due to the life-threatening nature of VF. Here’s an overview of the primary treatments:
1. Cardiopulmonary Resuscitation (CPR):
- Immediate Action: Begin CPR immediately if VF is suspected. Chest compressions help maintain circulation and oxygenation until advanced medical help arrives.
2. Defibrillation:
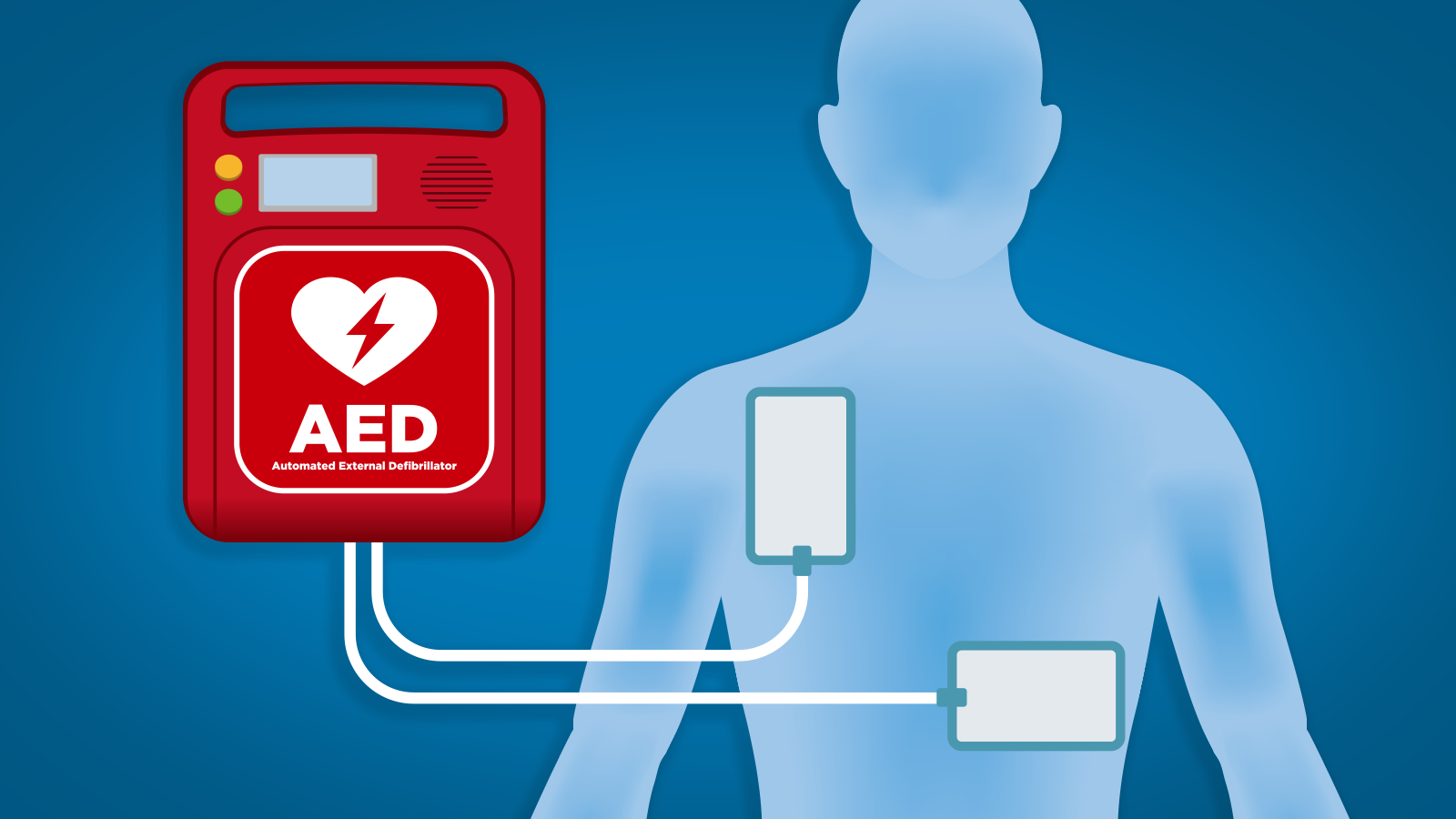
- Automated External Defibrillator (AED): An AED should be used as soon as possible to deliver a controlled electric shock to the heart. This can help restore a normal rhythm by interrupting the chaotic electrical activity causing VF.
- Manual Defibrillation: In a hospital setting, healthcare providers may use a manual defibrillator to administer shocks based on the patient’s specific condition and response.
3. Medications:
- Antiarrhythmic Drugs: Medications such as amiodarone or lidocaine may be administered to help stabilize the heart’s electrical activity and prevent recurrence of VF.
- Epinephrine: This medication may be given during CPR to help increase the chances of successful defibrillation and improve blood flow.
4. Advanced Cardiac Care:
- Cardiac Catheterization: If VF is due to coronary artery disease, angioplasty or stenting may be performed to open blocked arteries and restore blood flow.
- Coronary Artery Bypass Grafting (CABG): In some cases, surgical procedures may be necessary to address underlying heart disease.
5. Implantable Devices:
- Implantable Cardioverter-Defibrillator (ICD): For patients at high risk of recurring VF, an ICD may be implanted. This device monitors the heart’s rhythm and delivers shocks if VF occurs again.
6. Treating Underlying Conditions:
- Addressing Contributing Factors: Managing conditions such as coronary artery disease, electrolyte imbalances, or heart failure is crucial to preventing future episodes of VF.
7. Post-Resuscitation Care:
- Monitoring and Stabilization: After successful resuscitation, patients are closely monitored in an intensive care unit (ICU) or specialized cardiac unit. Further treatment may include medications, interventions to support heart function, and rehabilitation.
8. Lifestyle and Preventive Measures:
- Risk Factor Management: Addressing lifestyle factors such as smoking, diet, and exercise can help reduce the risk of future VF episodes.
- Follow-Up Care: Regular follow-up with a cardiologist to monitor heart health and adjust treatment plans as needed.
Immediate treatment is essential for survival and to minimize the risk of complications associated with VF. Prompt action by bystanders, along with advanced medical interventions, plays a critical role in improving outcomes.
Leave a Reply
You must be logged in to post a comment.