What are the symptoms of uterus didelphys?
Uterus didelphys is a rare congenital condition where a woman has two separate uteruses, each with its own cervix and sometimes a double vagina. The symptoms can vary, but common signs and issues associated with uterus didelphys include:
- Menstrual Irregularities: Heavy or painful periods, irregular bleeding, or more frequent menstruation due to the presence of two uteruses.
- Pelvic Pain: Pain in the pelvic region, which can be due to the abnormal shape or structure of the uterus.
- Reproductive Challenges: Difficulty with conception, miscarriage, or preterm labor due to the structural abnormalities.
- Complications During Pregnancy: Increased risk of preterm birth, breech presentation, or complications related to the growth and positioning of the fetus.
- Discomfort or Pain During Intercourse: Possible discomfort due to the presence of two uteruses and/or vaginas.
- Abnormal Discharge: Unusual vaginal discharge, which may be related to the anatomical differences.
Some women with uterus didelphys may have no symptoms and may only discover the condition during an examination for other reproductive issues or during imaging studies for unrelated reasons.
What are the causes of uterus didelphys?
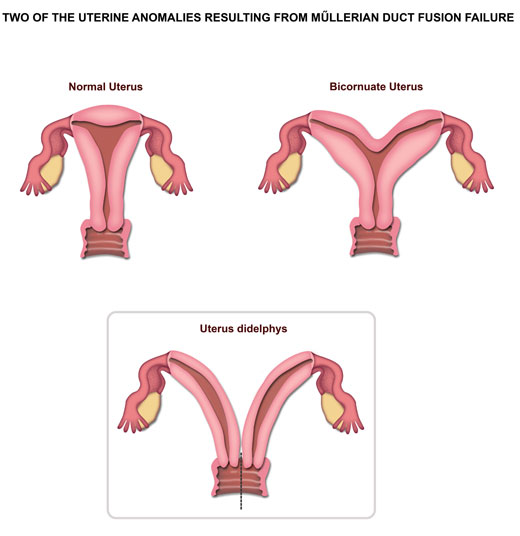
Uterus didelphys is caused by a developmental issue during embryonic development. Specifically, it results from the incomplete fusion of the Müllerian ducts, which are responsible for forming the uterus, cervix, and upper two-thirds of the vagina. Here are the key points regarding its causes:
- Embryonic Development: During fetal development, the Müllerian ducts normally fuse to form a single uterus. In the case of uterus didelphys, this fusion is incomplete, leading to the formation of two separate uterine cavities.
- Genetic Factors: While the exact cause is not always clear, there may be a genetic component influencing the development of uterine anomalies. However, a specific genetic cause for uterus didelphys has not been identified.
- Environmental Factors: Some research suggests that environmental factors or exposure to certain substances during pregnancy might affect the normal development of the Müllerian ducts, though this link is not well established.
- Random Developmental Anomalies: Often, the condition occurs sporadically without any known external causes, simply as a result of a random developmental anomaly.
In most cases, there is no known specific reason why the Müllerian ducts fail to fuse properly, and it is usually diagnosed incidentally during investigations for other gynecological issues.
What is the treatment for uterus didelphys?
The treatment for uterus didelphys focuses on managing symptoms and addressing complications rather than correcting the anatomical anomaly itself. Treatment strategies include:
- Regular Monitoring: Routine gynecological check-ups to monitor for any potential complications, such as infections or pregnancy-related issues.
- Management of Symptoms: Addressing any symptoms or complications, such as abnormal bleeding, pain, or pelvic discomfort, with appropriate medical interventions.
- Fertility Treatment: For women experiencing infertility or pregnancy complications, fertility treatments or assisted reproductive technologies (ART) may be considered. Options like intrauterine insemination (IUI) or in vitro fertilization (IVF) might be used, depending on individual circumstances.
- Pregnancy Care: Special care during pregnancy, including regular ultrasounds and monitoring for complications such as preterm labor or abnormal fetal positioning. Delivery may require a cesarean section (C-section) depending on the position of the fetus and other factors.
- Surgical Intervention: Surgery is generally not performed to correct the condition itself unless there are significant complications or associated conditions (such as large fibroids or severe pain) that require surgical intervention. In some cases, surgery might be considered to address specific issues like obstructed menstrual flow or to remove associated fibroids or polyps.
- Supportive Care: Providing emotional and psychological support, especially if the condition affects reproductive health or causes significant distress.
The approach is personalized based on the individual’s specific symptoms, reproductive plans, and overall health.
Leave a Reply
You must be logged in to post a comment.