What are the symptoms of undescended testicles?
The symptoms of undescended testicles (cryptorchidism) include:
- One or Both Testicles Not in the Scrotum: The primary sign is that one or both testicles are not felt in the scrotum where they normally should be. This can be noticed during a physical examination or by the absence of the testicles in the scrotum.
- Swelling or Pain: There may be swelling or pain in the groin area if the testicle is stuck in the groin or abdominal area.
- Abnormal Scrotum: The scrotum may appear smaller or less developed on the affected side.
- Asymmetry in the Scrotum: The scrotum may look uneven, with one side lacking a testicle or appearing less full.
- Visible Bulge: In some cases, there might be a bulge in the groin area where the undescended testicle is located.
- Infertility Issues: If left untreated, undescended testicles can lead to fertility problems later in life due to the higher temperatures in the abdomen affecting sperm production.
For infants, undescended testicles are often detected during a routine physical exam. It is important to follow up with a healthcare provider for further evaluation and management, as early treatment can help prevent complications and improve outcomes.
What are the causes of undescended testicles?
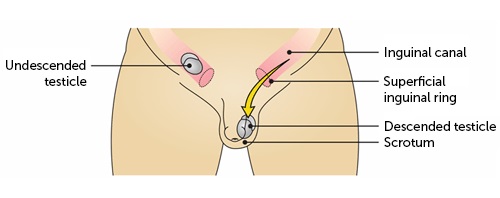
Undescended testicles, or cryptorchidism, occur when one or both testicles fail to move into the scrotum before birth. The causes can include:
- Hormonal Factors: Abnormalities in the hormones responsible for testicular descent, such as testosterone or other growth factors, can affect the proper movement of the testicles.
- Genetic Factors: Genetic conditions and family history can play a role. Some genetic disorders and congenital abnormalities increase the likelihood of undescended testicles.
- Premature Birth: Premature infants are more likely to have undescended testicles because the testicles may not have had enough time to descend into the scrotum before birth.
- Low Birth Weight: Infants with low birth weight may have a higher risk of having undescended testicles.
- Maternal Health Issues: Certain maternal health conditions, such as diabetes or other complications during pregnancy, can affect fetal development and increase the risk of undescended testicles.
- Anatomical Abnormalities: Structural issues within the abdomen or groin can interfere with the normal descent of the testicles.
- Environmental Factors: Some studies suggest that exposure to certain chemicals or environmental factors during pregnancy might contribute to undescended testicles, although more research is needed in this area.
It’s essential for undescended testicles to be monitored and treated appropriately to reduce the risk of complications, such as fertility issues or testicular cancer later in life.
What is the treatment for undescended testicles?
Treatment for undescended testicles typically involves surgical intervention, especially if the condition does not resolve on its own. Here’s a summary of the treatment options:
- Orchidopexy: The primary treatment is a surgical procedure called orchidopexy, which involves moving the testicle into its proper position in the scrotum and securing it there. This surgery is usually performed between 6 and 18 months of age, but it can be done later if needed.
- Hormonal Therapy: In some cases, hormone therapy with medications like human chorionic gonadotropin (hCG) or luteinizing hormone-releasing hormone (LHRH) may be used to stimulate the testicle to descend. This is less commonly used today due to variable success rates and potential side effects.
- Observation: In some instances, especially if the testicle is close to descending or if the child is very young, doctors may recommend a period of observation to see if the testicle will descend on its own before considering surgery.
- Follow-Up Care: After surgery or any other intervention, regular follow-up visits are important to ensure the testicle remains in place and to monitor for any potential complications.
Early intervention is crucial to reduce the risk of complications such as infertility, testicular cancer, and psychological issues related to body image.
Leave a Reply
You must be logged in to post a comment.