What are the symptoms of umbilical cord prolapse?
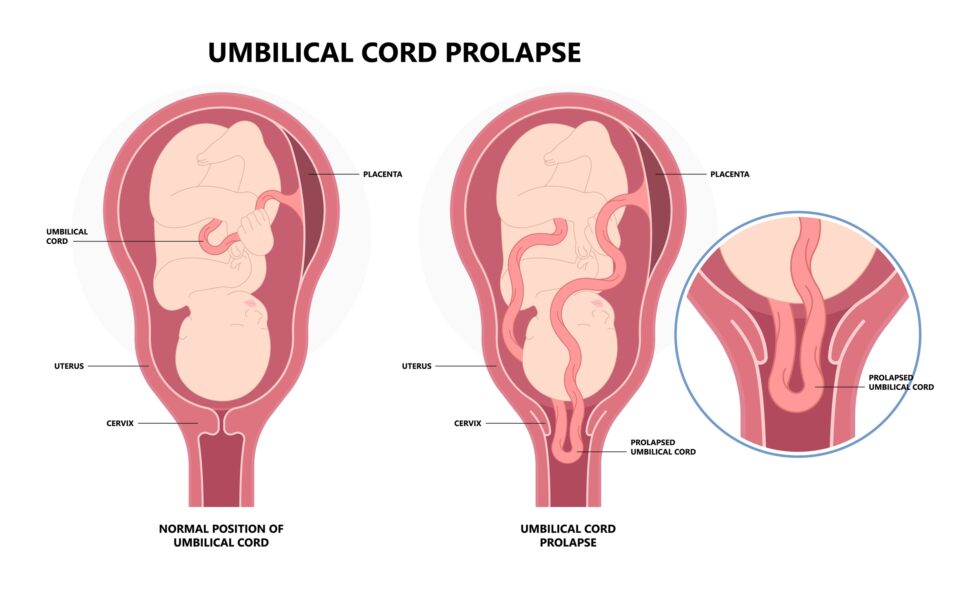
Umbilical cord prolapse occurs when the umbilical cord slips ahead of or alongside the presenting part of the fetus, which can compress the cord and reduce blood flow and oxygen to the baby. Symptoms and signs include:
- Fetal Heart Rate Abnormalities: The most common sign is a change in the fetal heart rate, often showing as a drop in the heart rate (bradycardia) or variable decelerations. This may be detected during routine fetal monitoring.
- Visible or Palpable Cord: In some cases, the prolapsed cord may be visible or palpable during a vaginal examination, particularly if it is outside the cervix.
- Decreased Fetal Movement: The mother might notice reduced fetal movement, which can be a sign of distress.
- Signs of Labor Complications: If the prolapse leads to severe fetal distress, it may cause signs such as abnormal uterine contractions or prolonged labor.
- Increased Risk of Complications: Umbilical cord prolapse is often associated with other complications such as premature rupture of membranes, a high birth weight baby, or an abnormal fetal presentation.
Early detection and prompt management are crucial to avoid serious outcomes, such as fetal hypoxia or acidosis. If umbilical cord prolapse is suspected, immediate medical attention is needed to manage the situation appropriately and ensure the safety of both mother and baby.
What are the causes of umbilical cord prolapse?
Umbilical cord prolapse occurs when the umbilical cord slips ahead of or alongside the presenting part of the fetus, which can lead to compression of the cord and reduced blood flow and oxygen to the baby. The causes and risk factors include:
- Abnormal Fetal Presentation: Breech or transverse fetal presentations can increase the likelihood of cord prolapse as the fetal presenting part may not engage fully in the pelvis.
- Premature Rupture of Membranes (PROM): When the membranes rupture early, there may be less cushioning around the fetus, increasing the risk of the cord slipping past the fetal head or body.
- Excessive Amniotic Fluid (Polyhydramnios): Excess fluid can cause excessive fetal movement and may lead to a higher risk of cord prolapse due to the increased space and mobility within the uterus.
- Multiple Gestations: In cases of twins or higher-order multiples, the increased number of fetal presentations can lead to abnormal positions and increased likelihood of cord prolapse.
- Long Umbilical Cord: A cord that is unusually long can have a higher chance of prolapsing, especially if there is more fetal movement or abnormal fetal presentation.
- High Birth Weight or Macrosomia: Larger babies may not engage properly in the pelvis, increasing the risk of cord prolapse.
- Uterine Anomalies or Abnormalities: Structural abnormalities in the uterus or the shape of the pelvis can contribute to a higher risk of cord prolapse.
- Excessive Manipulation During Labor: Maneuvers or excessive manual handling during labor can increase the risk of cord prolapse.
Addressing these risk factors when possible and careful monitoring during labor can help in managing and reducing the risk of umbilical cord prolapse.
What is the treatment for umbilical cord prolapse?
The treatment for umbilical cord prolapse involves immediate management to minimize the risk of fetal distress and ensure the well-being of both mother and baby. The approach typically includes:
- Immediate Manual Relief: If the prolapsed cord is detected, the healthcare provider will often attempt to relieve pressure on the cord manually. This involves gently pushing the presenting part of the fetus away from the cord to reduce compression.
- Change of Maternal Position: The mother may be positioned in various ways to help alleviate pressure on the umbilical cord. Positions such as the knee-chest position or Trendelenburg position (lying on the back with the legs elevated) may be used.
- Oxygen and Fluids: Providing supplemental oxygen to the mother and increasing intravenous fluids can help improve oxygenation and circulation to the fetus.
- Monitoring: Continuous fetal heart rate monitoring is essential to assess the baby’s well-being and detect any signs of distress.
- Emergency Delivery: If the fetal heart rate shows signs of distress that do not improve with conservative measures, an emergency delivery may be necessary. This could be through an instrumental delivery (forceps or vacuum extraction) or, more commonly, a cesarean section to quickly deliver the baby and relieve cord compression.
- Avoiding Further Manipulation: If possible, efforts will be made to avoid excessive manual handling or manipulation that could worsen the cord prolapse.
The specific management approach will depend on the clinical situation, including the stage of labor, the extent of fetal distress, and the overall health of the mother and baby. The goal is to ensure the safest outcome for both.
Leave a Reply
You must be logged in to post a comment.