What are the symptoms of a subchorionic hematoma?
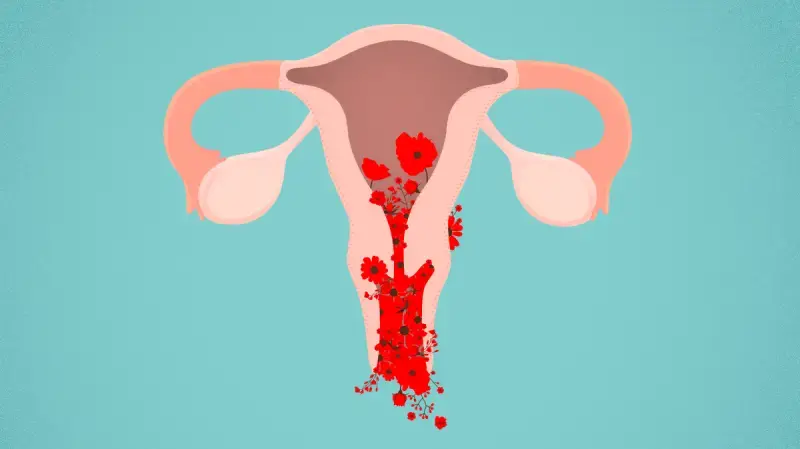
A subchorionic hematoma (SCH) is a type of bleeding that occurs between the uterine wall and the chorionic membrane during early pregnancy. The symptoms of a subchorionic hematoma can vary, but common signs include:
Vaginal Bleeding
- Spotting or Light Bleeding: This may be noticed as light pink or brown spotting.
- Heavy Bleeding: In some cases, bleeding can be more substantial, similar to a menstrual period.
Cramping
- Mild to Moderate Cramping: Some women experience cramping or discomfort in the lower abdomen, which can accompany the bleeding.
Pelvic Pain
- Localized Pain: Pain or discomfort in the pelvic area can occur, although it is often less severe compared to other types of bleeding.
Asymptomatic Cases
- No Symptoms: Some women with a subchorionic hematoma may not have any noticeable symptoms and the condition may be discovered incidentally during an ultrasound.
Ultrasound Findings
- Ultrasound Appearance: A subchorionic hematoma is typically detected through an ultrasound, which will show a blood collection between the uterine wall and the chorion.
While a subchorionic hematoma can cause anxiety due to the bleeding, it is often managed conservatively and may resolve on its own. However, if you experience any bleeding or cramping during pregnancy, it’s important to consult with a healthcare provider for a proper diagnosis and to rule out other potential issues.
What are the causes of a subchorionic hematoma?
A subchorionic hematoma (SCH) is a type of bleeding that occurs between the uterine wall and the chorionic membrane during early pregnancy. The exact cause of a subchorionic hematoma is not always clear, but several factors can contribute to its development:
Implantation
- Early Pregnancy Changes: The most common cause of a subchorionic hematoma is the implantation of the embryo into the uterine lining. This process can sometimes lead to bleeding if the embryo attaches in a way that causes a small tear or separation between the uterine wall and the chorion.
Uterine Abnormalities
- Anatomic Variations: Abnormalities in the shape or structure of the uterus, such as a septate uterus or fibroids, can increase the risk of subchorionic hematoma by affecting how the placenta attaches.
Hormonal Factors
- Hormonal Fluctuations: Changes in hormone levels, particularly those related to pregnancy, may influence the likelihood of bleeding or hematoma formation.
Trauma
- Physical Trauma: Although less common, physical trauma or injury to the abdomen can lead to bleeding and formation of a hematoma.
Chronic Conditions
- Underlying Health Issues: Certain chronic conditions, such as autoimmune disorders or clotting disorders, may be associated with an increased risk of bleeding and hematomas during pregnancy.
Pregnancy-Related Complications
- Multiple Pregnancies: Women carrying multiples (twins, triplets, etc.) may have a higher risk of subchorionic hematomas due to the increased stretching and stress on the uterine lining.
Placental Issues
- Placental Abnormalities: Problems with the placenta, such as placental abruption (where the placenta detaches prematurely from the uterine wall), can sometimes lead to bleeding and hematoma formation.
In many cases, a subchorionic hematoma resolves on its own as the pregnancy progresses, especially if it is small and there are no other complications. Regular monitoring by a healthcare provider is important to ensure the health of both the mother and the baby. If you experience any bleeding or discomfort during pregnancy, it’s essential to consult with a healthcare provider for an accurate diagnosis and appropriate care.
What is the treatment for a subchorionic hematoma?
The treatment for a subchorionic hematoma (SCH) typically focuses on managing symptoms, monitoring the condition, and ensuring the health of both the mother and the baby. Here are the general approaches to treatment:
Observation and Monitoring
- Regular Ultrasound: Frequent ultrasounds may be used to monitor the size of the hematoma and ensure that it is not growing or causing complications.
- Tracking Symptoms: Monitoring any symptoms, such as bleeding or cramping, to assess the progress of the hematoma and the overall health of the pregnancy.
Lifestyle and Activity Modifications
- Rest: In some cases, rest or reduced physical activity may be recommended, especially if bleeding is significant or if there are concerns about the risk of miscarriage.
- Avoiding Strenuous Activity: Limiting activities that could exacerbate bleeding or put additional stress on the body, such as heavy lifting or vigorous exercise.
Medications
- No Specific Medications: There are no specific medications to treat a subchorionic hematoma itself. However, medications may be prescribed to manage symptoms such as pain or cramping, if necessary.
Follow-Up Care
- Regular Check-Ups: Continued follow-up with a healthcare provider to ensure that the hematoma is not causing complications and to monitor the health of the pregnancy.
Emergency Care
- Seeking Medical Attention: If there is heavy bleeding, severe pain, or other concerning symptoms, it is important to seek immediate medical care to rule out more serious complications.
Addressing Complications
- Managing Potential Risks: If complications arise, such as a significant increase in bleeding or signs of preterm labor, more intensive interventions or treatments may be required based on the specific circumstances.
In many cases, a subchorionic hematoma resolves on its own as the pregnancy progresses. The majority of women with a SCH have normal pregnancies and deliveries. However, regular communication with a healthcare provider is crucial to ensure appropriate care and to address any concerns that may arise during the course of the pregnancy.
Leave a Reply
You must be logged in to post a comment.