What are the symptoms of spinal stenosis?
Spinal stenosis can cause a variety of symptoms depending on the location and severity of the narrowing in the spinal canal. Common symptoms include:
- Back Pain: Often a dull, aching pain that may worsen with activity or standing for long periods.
- Leg Pain: Pain, cramping, or weakness in the legs that typically worsens with walking or standing and improves with sitting or bending forward.
- Numbness and Tingling: Sensations of numbness, tingling, or pins-and-needles in the legs, buttocks, or feet.
- Weakness: Weakness in the legs or feet, which can affect balance and coordination.
- Walking Difficulties: Difficulty walking or a feeling of heaviness in the legs, which can limit mobility.
- Bladder Dysfunction or Bowel Dysfunction: In severe cases, problems with bladder or bowel control may occur.
Symptoms may vary and can develop gradually over time. In some cases, they may be exacerbated by certain activities or positions, such as standing for extended periods or walking long distances.
What are the causes of spinal stenosis?
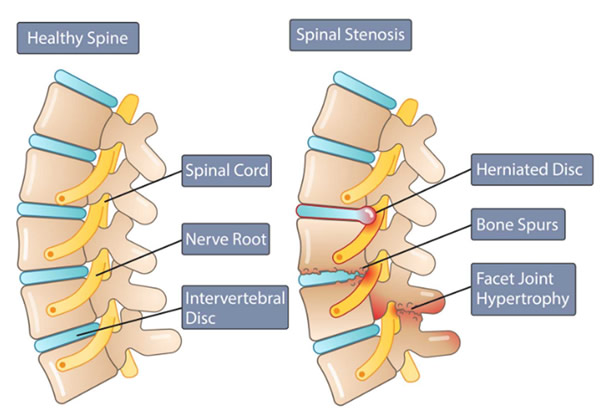
Spinal stenosis occurs when the spinal canal, which houses the spinal cord and nerves, becomes narrowed, leading to pressure on the spinal cord or nerve roots. The causes of spinal stenosis include:
- Degenerative Changes: Age-related changes in the spine, such as the degeneration of spinal discs, the formation of bone spurs, and thickening of the ligaments, can narrow the spinal canal. This is the most common cause and often results from osteoarthritis.
- Herniated Discs: When the soft inner material of a spinal disc bulges out through a tear in the outer layer, it can press against the spinal cord or nerve roots.
- Spinal Injuries: Trauma to the spine, such as fractures or dislocations, can lead to spinal stenosis by causing structural changes or displacement of spinal elements.
- Congenital Conditions: Some people are born with a naturally narrower spinal canal or other structural abnormalities that can predispose them to spinal stenosis.
- Spinal Tumors: Tumors within or near the spinal canal can take up space and compress the spinal cord or nerve roots.
- Ligamentum Flavum Thickening: The ligamentum flavum, which runs along the back of the spinal canal, can thicken and contribute to narrowing of the canal, especially in older adults.
- Paget’s Disease: This condition causes abnormal bone growth that can lead to spinal stenosis.
- Rheumatoid Arthritis: This autoimmune condition can cause inflammation in the spine, leading to joint damage and narrowing of the spinal canal.
These factors can contribute individually or in combination to the development of spinal stenosis.
How is the diagnosis of spinal stenosis made?
The diagnosis of spinal stenosis typically involves several steps and diagnostic tools:
- Medical History: The doctor will review the patient’s medical history, including any symptoms such as pain, numbness, weakness, or difficulty walking, and discuss any previous injuries or conditions.
- Physical Examination: The doctor will conduct a physical exam to assess the patient’s range of motion, strength, and reflexes. They may also check for signs of nerve compression, such as changes in sensation or muscle strength.
- Imaging Studies:
- X-rays: These can show changes in the bones of the spine, such as bone spurs, disc degeneration, and misalignment.
- Magnetic Resonance Imaging (MRI): MRI is particularly useful for visualizing soft tissues, including the spinal cord, discs, and ligaments. It can reveal the extent of canal narrowing, disc herniation, and any nerve root compression.
- Computed Tomography (CT) Scan: CT scans provide detailed cross-sectional images of the spine and can help identify bone spurs and other structural changes.
- CT Myelogram: This involves injecting a contrast dye into the spinal canal before taking CT scans, which can provide additional detail about spinal cord and nerve root compression.
- Electromyography (EMG) and Nerve Conduction Studies: These tests measure the electrical activity of muscles and nerves, helping to assess the function of the nerves affected by spinal stenosis.
- Other Diagnostic Tests: In some cases, additional tests such as a bone scan or discography may be used to further evaluate the condition.
The combination of clinical evaluation and imaging studies helps to confirm the diagnosis of spinal stenosis and determine the appropriate treatment plan.
What is the treatment for spinal stenosis?
The treatment for spinal stenosis varies depending on the severity of symptoms and the extent of spinal cord or nerve root compression. Treatment options include:
- Non-Surgical Treatments:
- Medications: Pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen can help manage pain. In some cases, corticosteroids may be prescribed to reduce inflammation.
- Physical Therapy: Exercises and stretches can strengthen the muscles supporting the spine, improve flexibility, and enhance overall function. Physical therapy may also help with posture correction and pain management.
- Lifestyle Modifications: Weight management, activity modifications, and ergonomic adjustments to daily activities can reduce strain on the spine and alleviate symptoms.
- Epidural Steroid Injections: These injections can provide temporary relief by reducing inflammation and swelling around the spinal nerves.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help relieve pain and reduce inflammation.
- Surgical Treatments: If non-surgical treatments are ineffective and symptoms significantly impact quality of life, surgical options may be considered:
- Laminectomy: This procedure involves removing part of the vertebra called the lamina to create more space for the spinal cord and nerves.
- Foraminotomy: This surgery enlarges the foramina (the openings where nerves exit the spinal canal) to relieve nerve compression.
- Discectomy: Removing a herniated or degenerated disc that is pressing on the spinal nerves or cord.
- Spinal Fusion: In some cases, fusion of the vertebrae may be performed to stabilize the spine after decompression surgery.
- Interspinous Process Decompression (IPD): A device is implanted to relieve pressure on the spinal nerves.
The choice of treatment depends on factors such as the patient’s overall health, the severity of the stenosis, and the impact on daily activities. A healthcare provider will work with the patient to develop an individualized treatment plan.
Leave a Reply
You must be logged in to post a comment.