What are the symptoms of schizoid personality disorder?
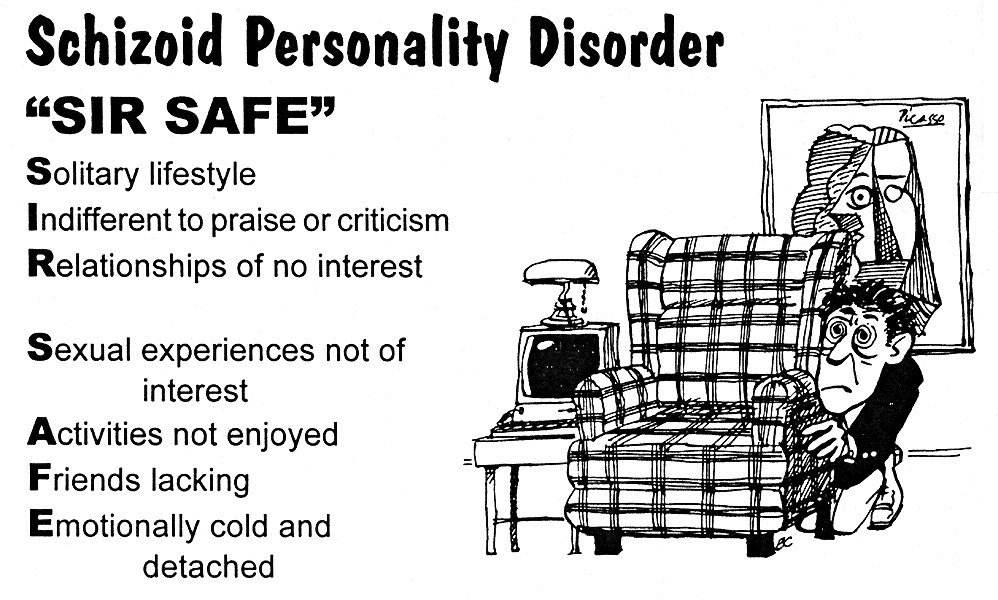
Schizoid personality disorder (SPD) is characterized by a pattern of detachment from social relationships and a limited range of emotional expression in interpersonal settings. Individuals with SPD often exhibit the following symptoms:
- A preference for being alone and choosing solitary activities
- Little or no interest in forming close relationships, including with family members
- Limited desire for sexual experiences with others
- A lack of close friends or confidants outside of immediate family
- Indifference to praise or criticism from others
- Emotional coldness, detachment, or flattened affectivity (limited emotional expression)
- Difficulty experiencing pleasure in most activities, leading to a tendency to appear indifferent or aloof
- A general lack of motivation or ambition, often appearing as if they have little interest in life
People with schizoid personality disorder often appear as loners or introverts, and they may be perceived as distant, indifferent, or lacking in empathy by others. They generally do not seek out social interactions and may prefer to engage in activities that require minimal social contact.
What are the causes of schizoid personality disorder?
The exact causes of schizoid personality disorder (SPD) are not fully understood, but it is believed to result from a combination of genetic, environmental, and psychological factors. Some of the possible contributing factors include:
- Genetics: A family history of personality disorders, particularly schizoid personality disorder or other related disorders like schizophrenia, may increase the risk of developing SPD. Genetic factors are thought to play a role in the development of the disorder, although the specific genes involved have not been identified.
- Childhood Environment: Early life experiences, such as emotional neglect, a lack of warmth or affection, or an environment that is emotionally cold or unresponsive, may contribute to the development of schizoid traits. Children who grow up in such environments might learn to detach emotionally as a coping mechanism.
- Psychological Factors: Certain personality traits or temperamental characteristics, such as a natural tendency towards introversion, may predispose individuals to develop SPD. These traits can be amplified by environmental factors or life experiences.
- Neurological Factors: There is some evidence to suggest that abnormalities in brain structure or function, particularly in areas involved in emotion and social interaction, could contribute to the development of schizoid personality disorder. However, more research is needed to confirm this.
Overall, the development of schizoid personality disorder is likely influenced by a combination of these factors, rather than a single cause.
How is the diagnosis of schizoid personality disorder made?
The diagnosis of schizoid personality disorder (SPD) is typically made through a comprehensive evaluation by a mental health professional, such as a psychiatrist or psychologist. The diagnostic process involves several steps:
- Clinical Interview: The mental health professional conducts a detailed interview with the individual, asking about their personal history, behavior patterns, thoughts, feelings, and relationships. The goal is to understand the individual’s overall mental health and specific symptoms.
- Observation of Behavior: The clinician may observe the individual’s behavior, particularly their social interactions and emotional responses. People with SPD often display limited emotional expression and may seem detached or indifferent in social situations.
- Psychological Assessment: Standardized psychological tests or questionnaires may be used to assess personality traits and identify characteristics associated with SPD. These tools help to gather more objective data about the individual’s personality and functioning.
- Diagnostic Criteria: The clinician compares the individual’s symptoms and behavior against the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the International Classification of Diseases (ICD-11). According to the DSM-5, SPD is diagnosed when a person exhibits a persistent pattern of detachment from social relationships and a restricted range of emotional expression in interpersonal settings.
- Exclusion of Other Conditions: The clinician rules out other mental health conditions that may have similar symptoms, such as depression, autism spectrum disorder, or other personality disorders. It’s important to distinguish SPD from these conditions to ensure an accurate diagnosis.
- Consideration of Functional Impact: The diagnosis also considers the extent to which the symptoms affect the individual’s daily life, relationships, and ability to function in social, occupational, or other areas.
A thorough evaluation is essential for accurately diagnosing schizoid personality disorder, as its symptoms can be subtle and may overlap with other mental health conditions.
What is the treatment for schizoid personality disorder?
The treatment for schizoid personality disorder (SPD) focuses on helping individuals manage symptoms and improve their quality of life, particularly in social functioning and emotional expression. Since people with SPD often do not seek treatment on their own, therapy is usually more effective when individuals are motivated and engaged in the process. Treatment options include:
1. Psychotherapy: The primary treatment for SPD is psychotherapy, specifically cognitive-behavioral therapy (CBT) or psychodynamic therapy. CBT helps individuals identify and change negative thought patterns and behaviors, while psychodynamic therapy focuses on exploring underlying emotional issues. Therapy may help individuals develop better social skills, improve their ability to form relationships, and increase emotional expression.
2. Social Skills Training: Social skills training can be beneficial in helping individuals with SPD learn and practice communication and interpersonal skills. This training often involves role-playing and other exercises to help individuals become more comfortable in social situations.
3. Group Therapy: Group therapy can provide a supportive environment where individuals with SPD can interact with others who may have similar experiences. This setting can help reduce feelings of isolation and provide opportunities to practice social interactions in a controlled environment.
4. Medication: While there is no specific medication to treat SPD, medications may be prescribed to address symptoms such as anxiety or depression if they are present. Antidepressants or antianxiety medications can help manage these co-occurring conditions.
5. Supportive Therapy: Supportive therapy focuses on providing encouragement and practical advice to help individuals cope with daily life challenges. This type of therapy can help build self-esteem and provide a sense of structure.
6. Lifestyle Adjustments: Encouraging lifestyle changes, such as engaging in regular physical activity, developing hobbies, and participating in structured social activities, can also help improve overall well-being.
Treatment for SPD can be challenging due to the nature of the disorder, as individuals may prefer solitude and have difficulty forming therapeutic relationships. However, with consistent and tailored therapeutic approaches, individuals with SPD can achieve improvements in their social functioning and emotional well-being.
Leave a Reply
You must be logged in to post a comment.