What are the symptoms of psoas syndrome?
Psoas syndrome, a condition related to the psoas muscle, often presents with a range of symptoms. Key symptoms include:
- Lower Back Pain: Pain is typically felt in the lower back, especially in the lumbar region.
- Hip Pain: Discomfort may extend to the hip joint.
- Groin Pain: Pain or tenderness might be experienced in the groin area.
- Difficulty with Movement: Activities involving hip flexion, such as walking or climbing stairs, may be painful or challenging.
- Stiffness: There might be stiffness in the lower back or hip region.
- Postural Changes: Individuals may adopt abnormal postures to alleviate pain, potentially leading to further discomfort.
- Referred Pain: Pain can sometimes radiate to the thigh or buttocks.
These symptoms are often exacerbated by prolonged sitting, heavy lifting, or specific movements. Diagnosis usually involves a combination of medical history, physical examination, and sometimes imaging studies.
What are the causes of psoas syndrome?
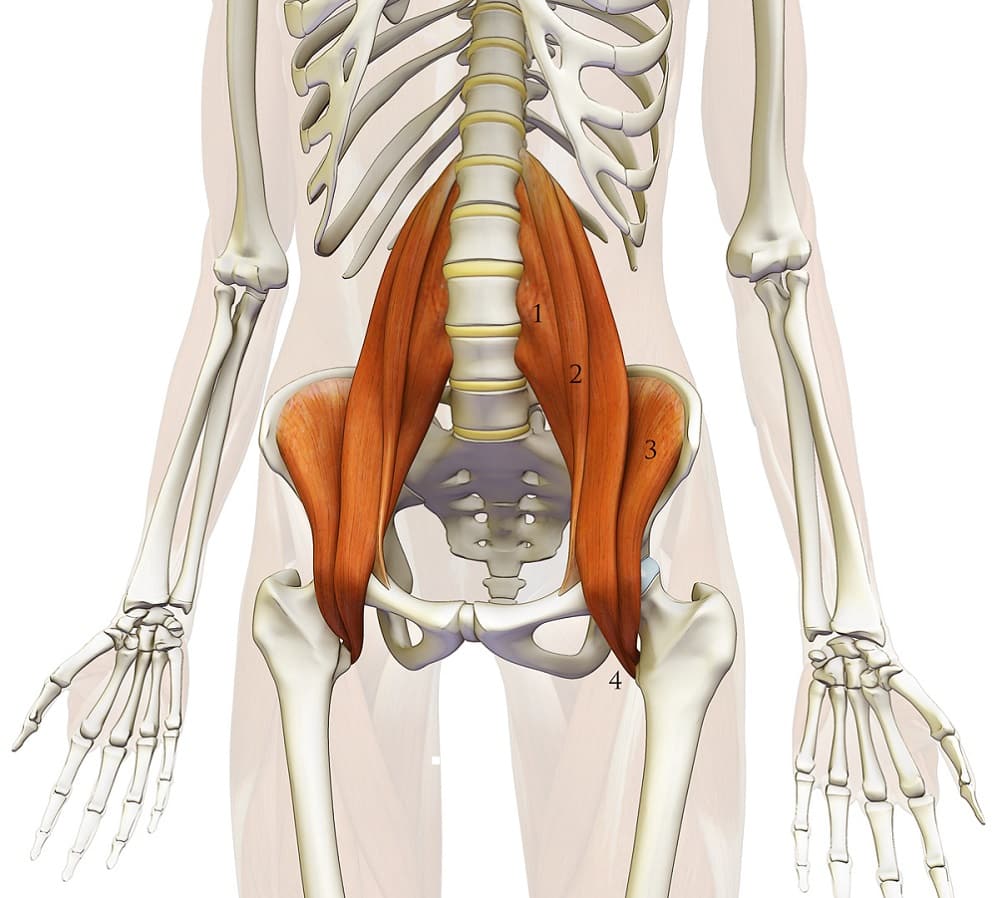
Psoas syndrome is primarily caused by irritation or dysfunction of the psoas muscle, which is a major muscle involved in hip flexion. The main causes include:
- Muscle Strain or Overuse: Activities that involve repetitive hip flexion or overuse, such as prolonged sitting or heavy lifting, can strain the psoas muscle.
- Poor Posture: Prolonged poor posture, especially sitting with poor lumbar support, can lead to muscle imbalances and strain.
- Sedentary Lifestyle: Lack of physical activity can lead to weakening and shortening of the psoas muscle, making it more susceptible to strain.
- Trauma or Injury: Direct trauma to the abdomen or lower back, such as from a fall or accident, can irritate or damage the psoas muscle.
- Imbalance in Core Muscles: Weakness or imbalance in surrounding core muscles, such as the abdominals and lower back muscles, can affect the psoas muscle’s function.
- Structural Abnormalities: Anatomical issues, such as an abnormal curvature of the spine (lordosis) or leg length discrepancies, can place additional stress on the psoas muscle.
- Inflammatory Conditions: Conditions like arthritis or inflammatory diseases can contribute to psoas dysfunction by affecting joint and muscle function.
Managing these factors through exercise, proper posture, and addressing any underlying conditions is crucial for alleviating psoas syndrome.
How is the diagnosis of psoas syndrome made?
Diagnosing psoas syndrome typically involves a detailed clinical evaluation and a series of diagnostic tests. The process starts with taking a thorough medical history and assessing symptoms, focusing on the nature of the pain, its location (often in the lower back, hip, or groin), onset, and any activities that may worsen it. During the physical examination, the healthcare provider checks for tenderness, spasm, and range of motion in the psoas muscle, often using specific tests like the Thomas test to assess hip flexor tightness or the psoas test to evaluate muscle strain.
Imaging studies can assist in ruling out other conditions. X-rays are used to check for structural abnormalities or fractures, while MRI provides detailed images of soft tissues, including the psoas muscle and nearby structures. A CT scan may also be utilized to examine the abdomen and pelvis for any abnormalities.
In some cases, blood tests are ordered to rule out inflammatory or infectious conditions that might mimic or contribute to the symptoms. The healthcare provider will also consider other potential causes, such as herniated discs or arthritis, to ensure an accurate diagnosis of psoas syndrome.
What is the treatment for psoas syndrome?
The treatment for psoas syndrome aims to relieve pain, reduce inflammation, and restore normal muscle function. This often includes:
- Rest and Activity Modification: Avoiding activities that exacerbate symptoms and giving the muscle time to heal.
- Physical Therapy: Engaging in targeted exercises and stretches to strengthen and lengthen the psoas muscle, improve flexibility, and correct any muscle imbalances.
- Pain Management: Using nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen to manage pain and reduce inflammation. In some cases, corticosteroid injections may be used for more severe inflammation.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area to alleviate pain and reduce muscle tension.
- Posture and Ergonomics: Correcting poor posture and improving ergonomics, especially if the syndrome is related to prolonged sitting or poor body mechanics.
In more persistent cases, additional interventions such as muscle relaxants or injections may be considered, and rarely, surgical options might be explored if conservative treatments are ineffective.
Leave a Reply
You must be logged in to post a comment.