What are the symptoms of post-traumatic arthritis?
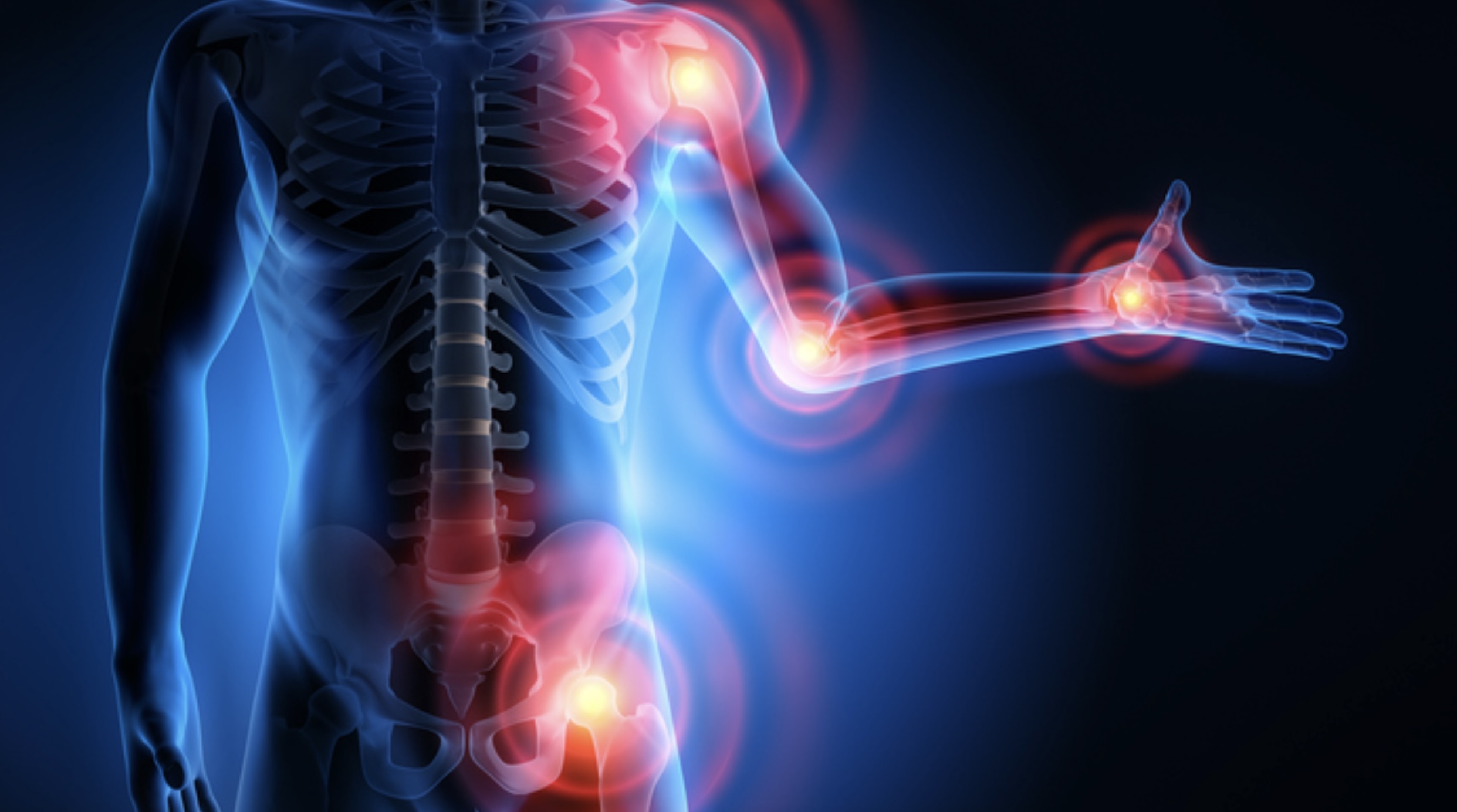
Post-traumatic arthritis is a type of arthritis that develops after an injury to a joint. The symptoms can vary depending on the severity of the injury and the extent of joint damage. Common symptoms include:
1. Joint Pain
- Persistent Pain: Ongoing pain in the affected joint, which may worsen with activity or weight-bearing.
2. Stiffness
- Reduced Mobility: Stiffness in the joint, especially after periods of inactivity or in the morning.
3. Swelling
- Edema: Swelling around the joint, which can lead to a visibly enlarged area.
4. Tenderness
- Sensitive to Touch: The joint may be tender to touch, and pressure on the joint can cause discomfort.
5. Decreased Range of Motion
- Limited Movement: Difficulty moving the joint through its full range of motion due to pain, stiffness, or mechanical obstruction.
6. Joint Warmth
- Increased Temperature: The affected joint may feel warm to the touch, indicating inflammation.
7. Crepitus
- Grinding Sensation: A grinding, popping, or crackling sensation in the joint when moving, due to roughened cartilage surfaces.
8. Functional Impairment
- Difficulty Performing Tasks: Challenges in performing daily activities or tasks that involve the affected joint, such as walking, gripping, or bending.
9. Inflammatory Symptoms
- Redness: Redness around the joint may occur if inflammation is significant.
10. Weakness
- Muscle Weakness: Weakness in the muscles surrounding the joint due to disuse or compensatory changes.
11. Joint Deformity
- Structural Changes: In severe cases, visible changes in joint shape or alignment may develop over time.
Post-traumatic arthritis often develops years after the initial injury, making it important to monitor joint health following significant joint trauma. If symptoms of post-traumatic arthritis arise, seeking medical evaluation and treatment can help manage the condition and improve quality of life.
What are the causes of post-traumatic arthritis?
Post-traumatic arthritis develops as a result of joint injury or trauma. The primary causes include:
1. Joint Injuries
- Fractures: Broken bones near or within a joint can disrupt the joint surface and lead to arthritis.
- Dislocations: Displacement of bones within a joint can damage the cartilage and surrounding structures.
- Ligament Injuries: Tears or sprains of ligaments that stabilize the joint can result in instability and subsequent arthritis.
2. Cartilage Damage
- Chondral Injuries: Direct damage to the cartilage, such as from an impact or abrasion, can impair the joint’s smooth movement and contribute to arthritis.
- Osteochondral Injuries: Damage that involves both the cartilage and underlying bone can lead to arthritis.
3. Repetitive Stress
- Chronic Overuse: Repeated stress or overuse of a joint, such as from certain sports or physical activities, can wear down cartilage and lead to arthritis over time.
4. Joint Surgery
- Post-Surgical Changes: Previous joint surgeries, such as those to repair fractures or torn ligaments, can alter joint mechanics and increase the risk of developing arthritis.
5. Previous Trauma
- Old Injuries: Previous joint trauma, even if it was not severe at the time, can contribute to arthritis years later as the joint undergoes gradual degeneration.
6. Inflammation
- Acute Inflammation: Initial inflammation following a joint injury can cause damage to cartilage and lead to arthritis.
7. Altered Joint Mechanics
- Misalignment: Injuries that affect the alignment of the joint can lead to uneven wear and tear, contributing to arthritis.
8. Genetic Factors
- Predisposition: Genetic factors may influence susceptibility to arthritis following joint injury.
9. Inadequate Rehabilitation
- Improper Healing: Inadequate or improper rehabilitation following a joint injury can lead to poor healing and increased risk of arthritis.
Post-traumatic arthritis is characterized by the gradual wearing away of cartilage and other joint structures due to the impact of injury or trauma. Effective management and treatment are essential to address the underlying causes and alleviate symptoms.
How is the diagnosis of post-traumatic arthritis made?
The diagnosis of post-traumatic arthritis is made through a combination of clinical evaluation, imaging studies, and sometimes laboratory tests. Here’s how the process generally unfolds:
1. Medical History and Physical Examination
- Patient History: The healthcare provider will ask about the patient’s symptoms, including pain, stiffness, swelling, and any history of joint injury or trauma.
- Physical Exam: The provider will examine the affected joint(s) for signs of swelling, tenderness, range of motion, and any mechanical issues. They may also check for signs of previous injuries or joint deformities.
2. Imaging Studies
- X-rays: X-rays are commonly used to visualize changes in bone structure and joint alignment. They can reveal joint space narrowing, bone spurs (osteophytes), and other signs of arthritis.
- MRI (Magnetic Resonance Imaging): MRI provides detailed images of both bone and soft tissues, including cartilage and ligaments. It helps assess the extent of cartilage damage and other internal joint structures.
- CT Scan (Computed Tomography): CT scans may be used to get detailed cross-sectional images of the joint and surrounding tissues, which can help in evaluating complex fractures or bone changes.
- Ultrasound: This imaging technique can be used to evaluate soft tissue structures, assess fluid in the joint, and guide diagnostic or therapeutic procedures.
3. Laboratory Tests
- Blood Tests: While not specific for post-traumatic arthritis, blood tests may be used to rule out other forms of arthritis or inflammatory conditions. They can help identify markers of inflammation or infection.
- Joint Aspiration: In some cases, a sample of synovial fluid from the joint may be analyzed to check for signs of infection, inflammation, or other abnormalities.
4. Arthroscopy
- Joint Inspection: In certain cases, an arthroscopy may be performed. This minimally invasive procedure involves inserting a small camera into the joint to directly visualize and assess the extent of cartilage damage and other joint issues.
5. Functional Assessment
- Impact on Function: The impact of symptoms on daily activities and joint function may be evaluated to understand the severity of the condition.
A comprehensive assessment combining these diagnostic approaches helps in accurately diagnosing post-traumatic arthritis and determining the appropriate treatment plan.
What is the treatment for post-traumatic arthritis?
The treatment for post-traumatic arthritis aims to manage symptoms, improve joint function, and slow disease progression. The approach can vary based on the severity of the condition and the specific joint affected. Here are the primary treatment strategies:
1. Medications
- Pain Relievers: Over-the-counter pain relievers like acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help alleviate pain and reduce inflammation.
- Corticosteroids: Oral or injected corticosteroids may be used for more severe inflammation to provide temporary relief.
- Topical Medications: Creams or gels containing NSAIDs or other anti-inflammatory agents can be applied directly to the affected joint.
2. Physical Therapy
- Exercise Programs: Tailored exercises can strengthen the muscles around the joint, improve flexibility, and maintain range of motion.
- Manual Therapy: Techniques such as joint mobilization may help improve joint function and reduce pain.
3. Lifestyle Modifications
- Weight Management: Maintaining a healthy weight can reduce stress on the affected joint and help alleviate symptoms.
- Activity Modification: Adjusting daily activities to avoid excessive strain on the joint can help manage pain and prevent further damage.
4. Assistive Devices
- Braces and Supports: Using joint braces, supports, or orthotic devices can provide stability and reduce strain on the affected joint.
- Mobility Aids: Devices such as canes or walkers can help improve mobility and reduce stress on the joints.
5. Injections
- Corticosteroid Injections: Injections into the joint can provide temporary relief from inflammation and pain.
- Hyaluronic Acid Injections: Also known as viscosupplementation, these injections can help lubricate the joint and improve function.
6. Surgical Interventions
- Arthroscopy: A minimally invasive procedure to clean out debris, repair damaged cartilage, or address other joint issues.
- Osteotomy: Surgical realignment of bones to redistribute weight and reduce joint stress.
- Joint Replacement: In cases of severe arthritis, partial or total joint replacement (arthroplasty) may be considered to restore joint function and alleviate pain.
7. Alternative Therapies
- Heat and Cold Therapy: Applying heat or cold to the joint can help manage pain and reduce inflammation.
- Acupuncture: Some individuals find relief through acupuncture, which involves inserting fine needles into specific points on the body.
8. Education and Support
- Patient Education: Learning about the condition, proper joint care, and pain management strategies can empower individuals to better manage their symptoms.
- Support Groups: Joining support groups or counseling can provide emotional support and practical advice from others with similar experiences.
Treatment plans for post-traumatic arthritis are individualized based on the patient’s specific needs and the severity of the condition. A multidisciplinary approach involving healthcare providers such as rheumatologists, orthopedic surgeons, physical therapists, and pain management specialists may be beneficial for comprehensive care.
Leave a Reply
You must be logged in to post a comment.