What are the symptoms of polyarthritis?
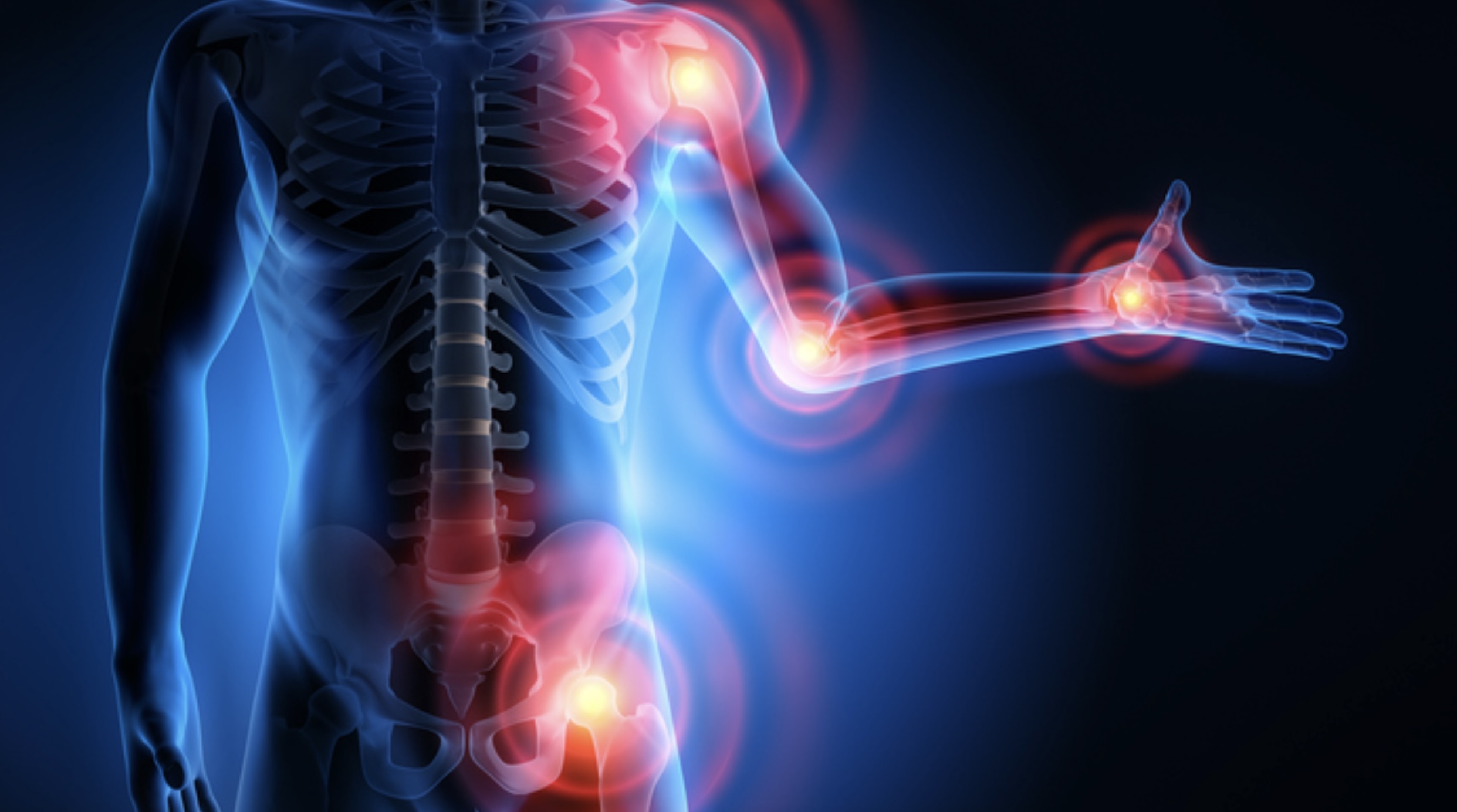
Polyarthritis is a condition characterized by inflammation in multiple joints. The symptoms can vary depending on the underlying cause but generally include:
1. Joint Symptoms
- Joint Pain: Affected joints may be painful, especially during movement.
- Swelling: Inflammation can cause swelling around the joints.
- Stiffness: Joints may feel stiff, particularly after periods of inactivity or in the morning.
- Redness: The skin over the affected joints may appear red and warm to the touch.
- Limited Range of Motion: Inflammation can reduce the ability to move the affected joints fully.
2. General Symptoms
- Fatigue: Generalized fatigue or a feeling of tiredness is common.
- Fever: Some forms of polyarthritis may be associated with fever.
- Weight Loss: Unexplained weight loss can occur, particularly in chronic or systemic forms of polyarthritis.
- General Malaise: A feeling of overall discomfort or illness.
3. Systemic Symptoms (Depending on the Underlying Cause)
- Skin Rash: Certain types of polyarthritis, like those associated with autoimmune diseases, may be accompanied by a rash.
- Eye Symptoms: Some forms may involve eye symptoms such as redness or pain.
- Organ Involvement: Inflammatory or autoimmune polyarthritis might affect other organs, leading to symptoms like shortness of breath or abdominal pain.
Types of Polyarthritis and Associated Symptoms
- Rheumatoid Arthritis: Symmetrical joint inflammation, morning stiffness lasting more than an hour, and systemic symptoms like fatigue and fever.
- Osteoarthritis: Typically affects weight-bearing joints, causing pain and stiffness with use.
- Psoriatic Arthritis: May present with skin psoriasis, nail changes, and dactylitis (swelling of fingers or toes).
- Reactive Arthritis: Follows an infection and may involve joints, eyes, and urinary tract.
- Gout: Severe pain and swelling, often affecting one joint at a time (such as the big toe) and associated with high uric acid levels.
Diagnosis and Evaluation
Diagnosis involves a detailed medical history, physical examination, and potentially additional tests such as blood work, imaging studies, or joint aspiration to determine the specific cause and tailor treatment accordingly. If you experience symptoms of polyarthritis, consulting with a healthcare provider for an accurate diagnosis and appropriate management is crucial.
What are the causes of polyarthritis?
Polyarthritis, or inflammation affecting multiple joints, can be caused by a variety of conditions. Here are some common causes:
1. Autoimmune Diseases
- Rheumatoid Arthritis: An autoimmune disorder that causes chronic inflammation in the joints.
- Systemic Lupus Erythematosus (SLE): An autoimmune disease that can cause joint pain along with other systemic symptoms.
- Psoriatic Arthritis: Associated with psoriasis and affects the joints and sometimes the spine.
- Juvenile Idiopathic Arthritis (JIA): An umbrella term for various types of arthritis in children.
2. Infectious Diseases
- Reactive Arthritis: Follows an infection, typically of the urogenital or gastrointestinal tract.
- Viral Arthritis: Caused by viruses such as parvovirus B19, hepatitis B or hepatitis C, and others.
- Bacterial Arthritis: Caused by bacterial infections that affect multiple joints, such as in cases of Lyme disease or gonococcal arthritis.
- Fungal Arthritis: Rare but can occur with fungal infections affecting the joints.
3. Metabolic Disorders
- Gout: Caused by the accumulation of uric acid crystals in the joints.
- Pseudogout (Calcium Pyrophosphate Deposition Disease): Caused by calcium pyrophosphate crystals in the joints.
4. Inflammatory Conditions
- Ankylosing Spondylitis: A form of arthritis that primarily affects the spine and can also involve peripheral joints.
- Behçet’s Disease: A rare disorder causing inflammation in various parts of the body, including joints.
5. Systemic Diseases
- Sarcoidosis: A disease characterized by the growth of small clusters of inflammatory cells in various organs, including the joints.
- Still’s Disease: A type of juvenile idiopathic arthritis with systemic symptoms, including fever and rash.
6. Other Causes
- Osteoarthritis: Typically affects individual joints but can sometimes affect multiple joints, especially in older adults.
- Trauma or Overuse: Repetitive stress or injury to joints can lead to inflammation and pain.
7. Drug-Induced Arthritis
- Medications: Certain medications can cause joint inflammation as a side effect.
8. Idiopathic
- Unknown Causes: In some cases, the cause of polyarthritis may not be clearly identified.
Diagnosis often requires a combination of clinical evaluation, laboratory tests, imaging studies, and sometimes joint aspiration or biopsy to identify the specific underlying cause and guide appropriate treatment. If you have symptoms of polyarthritis, consulting with a healthcare provider for a comprehensive assessment is important.
What is the treatment for polyarthritis?
The treatment for polyarthritis depends on the underlying cause, the severity of symptoms, and the specific joints affected. The general goals are to reduce inflammation, manage pain, preserve joint function, and address any underlying conditions. Here are the common approaches to treatment:
1. Medications
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Purpose: Reduce pain and inflammation.
- Examples: Ibuprofen, naproxen.
- Disease-Modifying Antirheumatic Drugs (DMARDs):
- Purpose: Slow disease progression, particularly in autoimmune forms.
- Examples: Methotrexate, sulfasalazine, hydroxychloroquine.
- Biologic Agents:
- Purpose: Target specific immune system pathways involved in inflammation.
- Examples: Tumor necrosis factor (TNF) inhibitors like etanercept or adalimumab, interleukin inhibitors like tocilizumab.
- Corticosteroids:
- Purpose: Quickly reduce inflammation and manage severe symptoms.
- Examples: Prednisone, injected corticosteroids for localized inflammation.
- Pain Relievers:
- Purpose: Manage pain without reducing inflammation.
- Examples: Acetaminophen (Tylenol).
2. Physical Therapy and Exercise
- Physical Therapy:
- Purpose: Improve joint function, strength, and flexibility.
- Approach: Tailored exercises and techniques to enhance joint movement and reduce stiffness.
- Exercise:
- Purpose: Maintain joint function, strengthen muscles around joints, and manage weight.
- Types: Low-impact exercises like swimming, cycling, and stretching.
3. Lifestyle Modifications
- Weight Management:
- Purpose: Reduce stress on weight-bearing joints.
- Approach: Balanced diet and regular exercise.
- Joint Protection:
- Purpose: Minimize joint strain and prevent further damage.
- Approach: Use assistive devices, practice good posture, and avoid repetitive strain.
4. Surgical Interventions
- Joint Injection:
- Purpose: Provide relief from inflammation and pain.
- Type: Corticosteroid injections directly into the affected joint.
- Joint Replacement Surgery:
- Purpose: Replace severely damaged joints with artificial ones.
- Examples: Hip or knee replacement.
- Arthroscopy:
- Purpose: Surgically inspect and treat joint damage.
- Approach: Minimally invasive technique to remove damaged tissue or repair joint structures.
5. Management of Underlying Conditions
- Infectious Causes:
- Purpose: Treat underlying infections with appropriate antibiotics or antiviral medications.
- Metabolic Disorders:
- Purpose: Manage conditions like gout with medications to lower uric acid levels or calcium pyrophosphate crystals.
6. Supportive Care
- Education and Counseling:
- Purpose: Provide information on managing the disease and coping strategies.
- Approach: Patient education on disease management, stress reduction techniques.
- Psychological Support:
- Purpose: Address mental health aspects of chronic illness.
- Approach: Counseling or support groups to cope with the impact of polyarthritis.
7. Regular Monitoring
- Follow-Up Care:
- Purpose: Monitor disease activity, medication side effects, and treatment effectiveness.
- Approach: Regular check-ups with healthcare providers and periodic laboratory tests.
Treatment plans are individualized based on the type of polyarthritis, the patient’s overall health, and specific needs. A multidisciplinary approach involving rheumatologists, physical therapists, and other specialists is often beneficial in managing polyarthritis effectively.
Leave a Reply
You must be logged in to post a comment.