What are the symptoms of pinta?
Pinta is a skin infection caused by the bacterium Treponema carateum, which is closely related to the bacteria responsible for syphilis. It is primarily found in tropical regions, particularly in parts of Central and South America.
Symptoms of Pinta
- Primary Lesion (Papule): The initial stage typically presents as a small, reddish or purplish papule (raised bump) that appears on the skin. This lesion usually develops in areas exposed to sunlight.
- Secondary Lesion (Plaque): Over time, the papule may enlarge and become a larger, flat, and discolored plaque. These plaques can be rough, scaly, or crusty and may have a lighter color compared to the surrounding skin.
- Skin Changes: The affected skin may show changes in pigmentation, with lesions varying from reddish-brown to grayish-white. The lesions can become more extensive and affect larger areas of the body.
- Itching or Discomfort: Pinta lesions may cause itching or mild discomfort, but they are generally not painful.
- Lack of Systemic Symptoms: Unlike some other infections, pinta usually does not cause systemic symptoms such as fever or malaise.
- Chronic Lesions: If untreated, pinta can lead to chronic skin lesions that may remain for years, potentially causing cosmetic concerns.
If you suspect you have pinta or have been in an area where it is common, it is important to seek medical evaluation for proper diagnosis and treatment.
What are the causes of pinta?
Pinta is caused by the bacterium Treponema carateum, a type of spirochete. This bacterium is related to the ones responsible for syphilis (Treponema pallidum) and yaws (Treponema pertenue). The primary factors contributing to the spread of pinta include:
- Direct Skin Contact: Pinta is transmitted through direct skin contact with lesions of an infected person. The bacteria enter through broken skin or abrasions.
- Poor Hygiene and Living Conditions: In areas with inadequate sanitation and hygiene, the risk of pinta is higher. Crowded living conditions and poor access to clean water and healthcare can facilitate the spread of the infection.
- Environmental Factors: Pinta is more common in tropical and subtropical regions, where conditions such as high humidity and exposure to sunlight may contribute to the development and persistence of skin lesions.
- Lack of Medical Resources: Limited access to healthcare and diagnostic resources can delay treatment and increase the risk of ongoing transmission and complications.
Pinta is not as widely spread as other treponemal infections like syphilis or yaws, but in endemic areas, it remains a concern. Preventive measures include improving hygiene practices, avoiding contact with infected individuals, and enhancing access to medical care.
What is the treatment for pinta?
Pinta is effectively treated with antibiotics. The standard treatment options include:
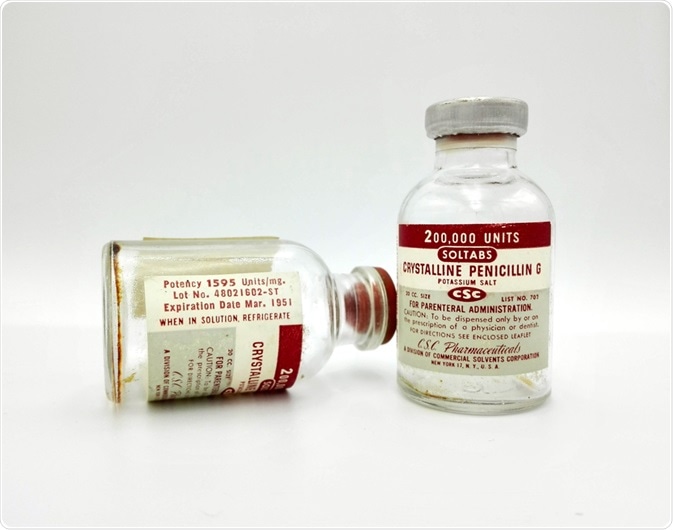
- Penicillin: This is the most commonly used antibiotic for treating pinta. It is usually administered as an intramuscular injection or orally, depending on the severity of the infection.
- Tetracyclines: For individuals who are allergic to penicillin or in areas where penicillin is not available, tetracyclines (such as doxycycline) can be used as an alternative treatment.
- Other Antibiotics: In some cases, other antibiotics like azithromycin may be used if penicillin or tetracyclines are not suitable.
Treatment Goals:
- Eliminate the Bacterium: The primary goal is to eradicate Treponema carateum from the body to resolve the skin lesions and prevent further spread.
- Improve Skin Lesions: Effective treatment should lead to the healing of skin lesions and improvement in pigmentation.
Follow-Up and Care:
- Monitor Progress: Follow-up care is important to ensure that the lesions are healing properly and to address any residual symptoms.
- Prevent Reoccurrence: Addressing factors that may contribute to the spread of the infection, such as improving hygiene and living conditions, is crucial to prevent reoccurrence.
Medical Consultation:
It’s important to consult a healthcare provider for proper diagnosis and treatment. They will determine the most appropriate antibiotic regimen based on the individual’s health condition and local medical practices.
Leave a Reply
You must be logged in to post a comment.