What are the symptoms of a pilonidal cyst?
A pilonidal cyst is a sac-like structure that can develop in the area near the tailbone, typically at the top of the buttocks crease. The symptoms of a pilonidal cyst can vary depending on whether it is infected or not. Here are common symptoms:
1. Pain and Discomfort:
- Localized Pain: Pain in the area near the tailbone, which may be sharp or throbbing.
- Discomfort: Pain can worsen when sitting or standing for prolonged periods.
2. Swelling and Redness:
- Swelling: The area may become swollen and tender to the touch.
- Redness: The skin over the cyst can become red and inflamed.
3. Drainage:
- Pus or Fluid: The cyst may drain pus, blood, or a clear fluid, which can be foul-smelling.
- Pilonidal Sinus Tracts: Small openings (sinus tracts) in the skin may discharge fluid.
4. Itching:
- Itchiness: The affected area may itch due to irritation or inflammation.
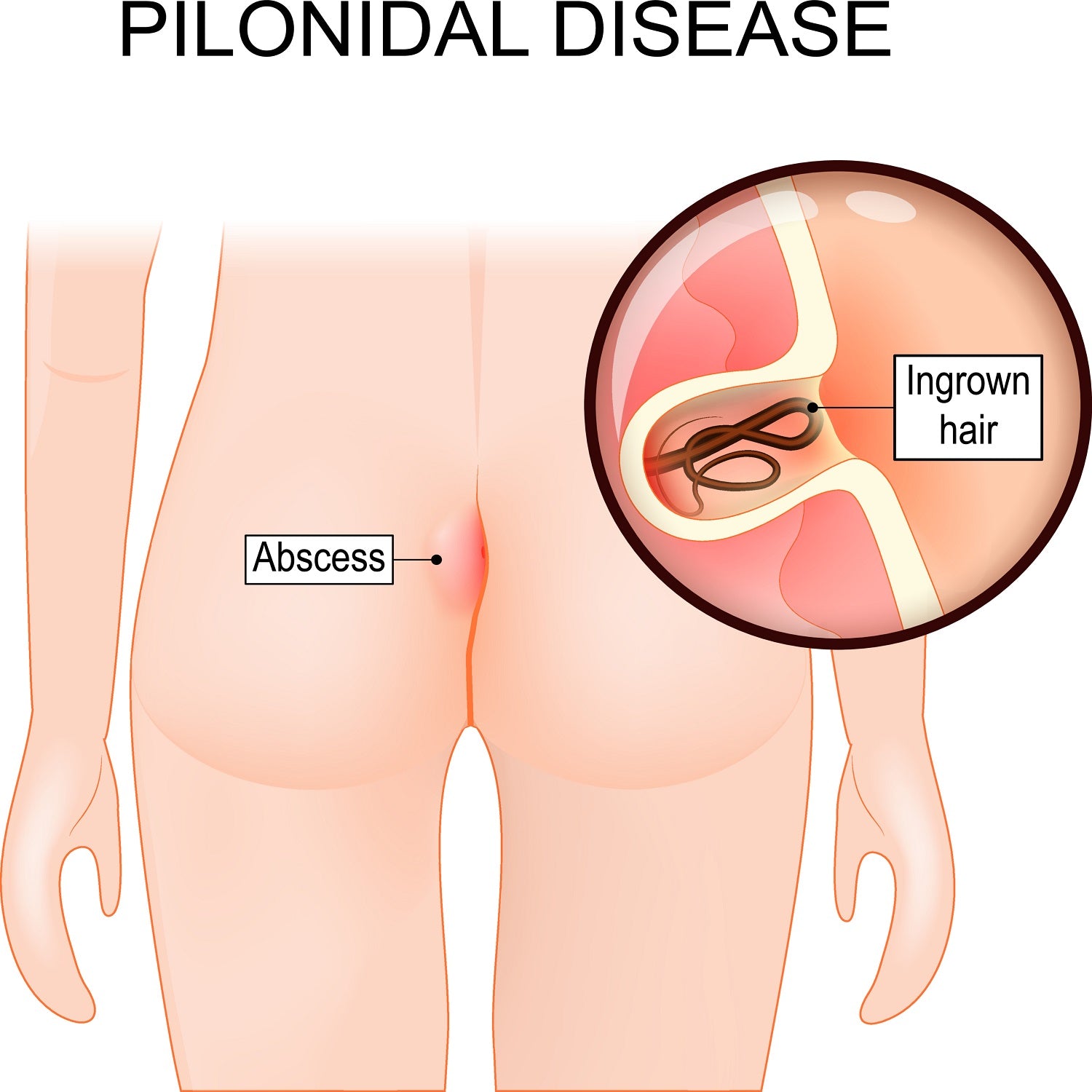
5. Abscess Formation:
- Abscess: In some cases, an infection can lead to the formation of an abscess, causing increased pain, swelling, and redness.
6. Fever (if infected):
- Systemic Symptoms: In cases of severe infection, systemic symptoms like fever and malaise may occur.
Summary:
Symptoms of a pilonidal cyst can include localized pain, swelling, redness, drainage of pus or fluid, itching, and, in cases of infection, fever. Early recognition and treatment can help manage symptoms and prevent complications. If you suspect you have a pilonidal cyst, especially if it becomes painful, swollen, or starts to drain, it is advisable to seek medical attention.
What are the causes of a pilonidal cyst?
The exact cause of a pilonidal cyst is not fully understood, but several factors are believed to contribute to its development. Here are the primary causes and risk factors:
1. Hair Follicle Issues:
- Hair Involvement: The cyst often forms near hair follicles in the skin. Ingrown hairs or hair growth that becomes trapped under the skin may contribute to cyst formation.
2. Skin Irritation and Trauma:
- Repeated Friction: Prolonged sitting, repetitive friction, or pressure in the area can irritate the skin and hair follicles, increasing the risk of cyst formation.
- Trauma: Physical trauma or injury to the area near the tailbone can also lead to the development of a pilonidal cyst.
3. Congenital Factors:
- Genetic Predisposition: Some individuals may be genetically predisposed to developing pilonidal cysts due to the structure of their hair follicles or skin.
4. Poor Hygiene:
- Hygiene Factors: Although not a direct cause, poor hygiene can contribute to the irritation and infection of pilonidal cysts. Accumulation of sweat, dirt, or bacteria can exacerbate the condition.
5. Hormonal Changes:
- Puberty: Pilonidal cysts are more common in adolescents and young adults, suggesting that hormonal changes during puberty might play a role.
6. Obesity:
- Excess Weight: Being overweight or obese can increase the risk of developing pilonidal cysts due to additional pressure and friction in the buttock area.
7. Sedentary Lifestyle:
- Prolonged Sitting: Individuals who sit for extended periods, such as those with sedentary jobs, may be at a higher risk due to increased pressure and friction on the area.
Summary:
Pilonidal cysts are believed to be caused by a combination of factors including hair follicle issues, skin irritation or trauma, genetic predisposition, poor hygiene, hormonal changes, obesity, and a sedentary lifestyle. These factors can contribute to the development of the cyst and its potential for infection and inflammation.
How is the diagnosis of a pilonidal cyst made?
The diagnosis of a pilonidal cyst is typically made based on a combination of clinical evaluation and sometimes imaging studies. Here’s how the diagnosis is usually made:
1. Medical History:
- Symptom Review: The healthcare provider will ask about symptoms such as pain, swelling, redness, and drainage in the area near the tailbone. They may also inquire about any history of trauma, irritation, or infection in the area.
2. Physical Examination:
- Inspection: The provider will examine the area around the tailbone for signs of a cyst, such as swelling, redness, and drainage. They will look for characteristic features like a small pit or sinus tract in the skin.
- Palpation: The area will be palpated (gently pressed) to assess tenderness, swelling, and the presence of any fluid or pus.
3. Diagnostic Imaging:
- Ultrasound: An ultrasound may be used to visualize the cyst and assess its size, depth, and any associated abscess formation. It can also help identify sinus tracts or fluid accumulation.
- CT Scan: In some cases, a CT scan may be used to get a detailed view of the cyst and surrounding structures, particularly if there is suspicion of a more complex infection or abscess.
- MRI: An MRI is less commonly used but may be considered if the cyst is particularly large or complex, or if there are concerns about deeper tissue involvement.
4. Laboratory Tests:
- Culture: If the cyst is infected and discharging pus, a sample may be taken for culture to identify any bacterial infection and determine the appropriate antibiotic treatment.
- Blood Tests: Although not typically required for diagnosis, blood tests may be done to check for signs of systemic infection or inflammation if needed.
Summary:
The diagnosis of a pilonidal cyst is primarily based on a physical examination and patient history, with additional imaging studies such as ultrasound or CT scans used to confirm the diagnosis and assess the extent of the cyst. Laboratory tests may be conducted if there is evidence of infection.
What is the treatment for a pilonidal cyst?
The treatment for a pilonidal cyst depends on the severity of the condition and whether there is an associated infection. The options range from conservative management to surgical intervention. Here’s an overview of common treatments:
1. Conservative Management:
- Antibiotics: If there is an infection, antibiotics may be prescribed to treat it. The choice of antibiotic will depend on the results of a culture if taken.
- Warm Compresses: Applying warm compresses to the area can help reduce inflammation and promote drainage of any pus.
- Pain Relief: Over-the-counter pain relievers like acetaminophen or ibuprofen can help alleviate discomfort.
2. Surgical Treatment:
- Incision and Drainage: If the cyst is infected and an abscess has formed, a healthcare provider may perform an incision and drainage procedure to remove the pus and relieve pressure.
- Excision: For chronic or recurrent pilonidal cysts, a surgical procedure may be needed to remove the cyst and any associated sinus tracts. There are different surgical techniques, including:
- Simple Excision: Removal of the cyst and surrounding tissue, with the wound left open to heal.
- Flap Surgery: Involves removing the cyst and covering the wound with a flap of nearby tissue to promote healing and reduce the risk of recurrence.
- Laser Treatment: Laser surgery may be used to remove the cyst and treat the affected area with minimal invasiveness.
- Closure: After removal, the wound may be closed with stitches or left open to heal by secondary intention, depending on the surgical approach and the extent of the removal.
3. Postoperative Care:
- Wound Care: Proper care of the wound is essential to prevent infection and promote healing. This may include keeping the area clean, changing dressings regularly, and avoiding activities that put pressure on the area.
- Follow-up: Regular follow-up with a healthcare provider is important to monitor healing and address any complications or recurrence.
4. Lifestyle and Preventive Measures:
- Hygiene: Maintaining good hygiene and avoiding prolonged sitting can help prevent recurrence.
- Weight Management: For individuals who are overweight, losing weight can reduce pressure and friction in the area.
Summary:
Treatment for a pilonidal cyst may involve antibiotics and warm compresses for mild cases, while more severe or recurrent cases often require surgical intervention. Postoperative care and lifestyle adjustments are crucial to ensure proper healing and prevent recurrence.
Leave a Reply
You must be logged in to post a comment.