What are the symptoms of pericoronitis?
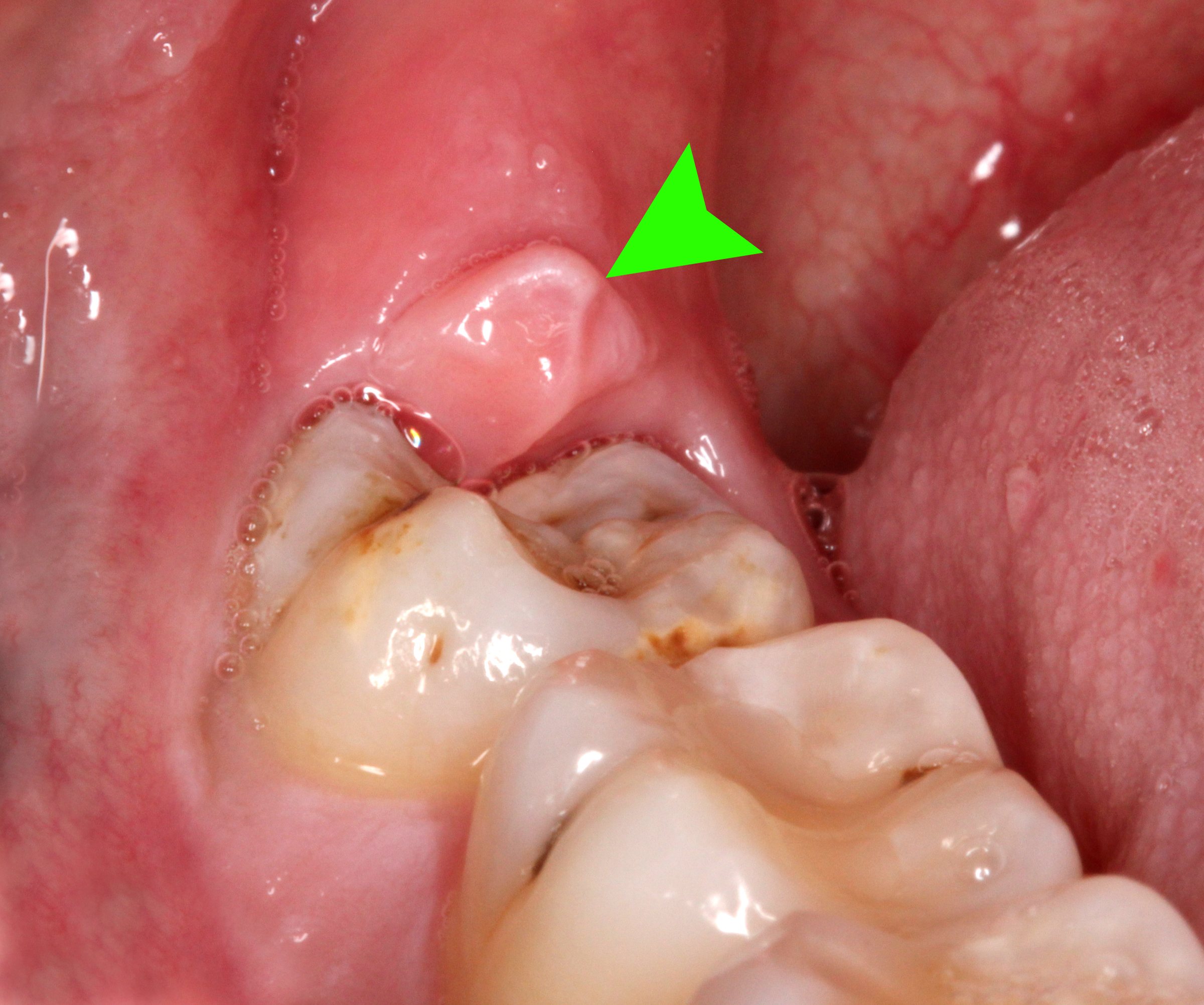
Pericoronitis is an inflammation of the gum tissue around the crown of a partially erupted or impacted tooth, commonly affecting the third molars (wisdom teeth). The symptoms of pericoronitis can vary in severity and may include:
1. Pain
- Localized Pain: Pain around the affected tooth or in the gum area.
- Radiating Pain: Pain that may radiate to the jaw, ear, or throat.
2. Swelling
- Gum Swelling: Swelling of the gum tissue around the partially erupted tooth.
- Localized or Generalized: The swelling can be localized to the area around the tooth or may spread to the surrounding tissues.
3. Redness and Warmth
- Inflammation: Redness and increased warmth in the gum tissue surrounding the tooth.
4. Discharge
- Pus: The presence of a foul-smelling discharge or pus from the gum area.
5. Difficulty Opening the Mouth
- Trismus: Limited ability to open the mouth fully due to pain and swelling.
6. Bad Breath
- Halitosis: Foul breath resulting from the infection and discharge.
7. Fever and Malaise
- Systemic Symptoms: In severe cases, symptoms such as fever and general malaise may occur.
8. Bad Taste
- Altered Taste: A bad or metallic taste in the mouth due to infection and discharge.
Summary
Symptoms of pericoronitis primarily include localized pain, swelling, redness, and discharge around the partially erupted tooth. Difficulty opening the mouth, bad breath, and systemic symptoms like fever may also occur in more severe cases. Prompt treatment is important to manage symptoms and prevent complications.
What are the causes of pericoronitis?
Pericoronitis is caused by inflammation of the gum tissue around the crown of a partially erupted or impacted tooth, often the third molars (wisdom teeth). The primary causes and contributing factors include:
1. Partial Eruption of the Tooth
- Incomplete Eruption: When a tooth does not fully emerge through the gum line, it creates a flap of gum tissue (operculum) that can trap food and bacteria.
2. Bacterial Infection
- Bacterial Growth: Accumulation of bacteria under the operculum or around the partially erupted tooth can lead to infection and inflammation.
3. Food and Debris Trapping
- Retention of Food: Food particles and debris can become trapped between the tooth and the gum tissue, providing a medium for bacterial growth.
4. Poor Oral Hygiene
- Inadequate Cleaning: Poor oral hygiene can exacerbate the buildup of plaque and bacteria around the partially erupted tooth, leading to infection.
5. Mechanical Irritation
- Toothbrush Injury: Aggressive brushing or use of a hard-bristled toothbrush can irritate the gum tissue.
- Food Particles: Hard or sticky foods that come into contact with the area can cause irritation.
6. Impacted Tooth
- Inadequate Space: An impacted tooth (one that is unable to erupt fully due to lack of space) can increase the risk of pericoronitis.
7. Immune System Factors
- Weakened Immunity: Individuals with compromised immune systems may be more susceptible to infections, including pericoronitis.
8. Systemic Conditions
- Underlying Health Issues: Certain health conditions that affect the immune system or oral health can contribute to the development of pericoronitis.
Summary
Pericoronitis is primarily caused by the partial eruption of a tooth, often exacerbated by bacterial infection, food and debris trapping, poor oral hygiene, and mechanical irritation. Impacted teeth and systemic factors can also play a role. Proper oral hygiene and timely dental care are important for preventing and managing pericoronitis.
How is the diagnosis of pericoronitis made?
Diagnosing pericoronitis typically involves a combination of clinical examination, patient history, and, if necessary, supplementary tests. Here’s how the diagnosis is generally made:
1. Medical History
- Patient History: The dentist will ask about symptoms, including pain, swelling, and any previous issues with the affected tooth or other dental problems.
- Symptom Review: Detailed information on the onset, duration, and severity of symptoms such as pain, swelling, and discharge.
2. Physical Examination
- Inspection: The dentist will examine the affected area, looking for signs of inflammation, redness, swelling, and discharge around the partially erupted tooth.
- Palpation: Gentle palpation of the gum tissue around the tooth to assess tenderness and to identify any swelling or pus.
- Evaluation of Tooth Eruption: Assessment of the position and eruption status of the tooth.
3. Diagnostic Tests
- Radiographic Imaging:
- Panoramic X-ray: Provides a comprehensive view of the teeth and surrounding structures to identify impacted teeth, assess the extent of the problem, and check for any damage or infection.
- Periapical X-ray: Focuses on the area around the tooth root to evaluate bone levels and detect any infection or abscess.
4. Differential Diagnosis
- Rule Out Other Conditions: The dentist will consider other conditions that may cause similar symptoms, such as abscesses, periodontal disease, or other oral infections, to confirm the diagnosis of pericoronitis.
Summary
The diagnosis of pericoronitis is primarily made through a thorough medical history and physical examination, with the aid of radiographic imaging to assess the tooth and surrounding structures. The dentist will evaluate symptoms and examine the affected area to confirm the presence of pericoronitis and rule out other potential conditions.
What is the treatment for pericoronitis?
Treatment for pericoronitis focuses on alleviating symptoms, addressing the infection, and preventing recurrence. The specific approach may vary depending on the severity of the condition. Here’s a general outline of treatment options:
1. Cleaning and Debridement
- Scaling and Polishing: Professional cleaning by a dentist to remove plaque and debris from around the affected tooth.
- Flushing: Rinsing the area with an antimicrobial solution to reduce bacterial load and clean the area.
2. Antibiotic Therapy
- Oral Antibiotics: Prescribed if there is significant infection or if the patient has systemic symptoms. Common options include amoxicillin, metronidazole, or clindamycin.
- Topical Antibiotics: In some cases, topical antibiotics or antiseptic gels may be applied directly to the affected area.
3. Pain Management
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation.
- Acetaminophen: For pain relief if NSAIDs are not suitable.
4. Surgical Intervention
- Operculectomy: Removal of the operculum (flap of gum tissue) to alleviate symptoms and allow for better cleaning and oral hygiene.
- Tooth Extraction: In cases where the affected tooth is severely impacted or recurrent problems occur, extraction of the tooth may be recommended to prevent future episodes.
5. Oral Hygiene and Self-Care
- Rinsing: Use of warm saltwater rinses or antimicrobial mouth rinses to help keep the area clean and reduce discomfort.
- Brushing: Proper brushing and flossing to maintain good oral hygiene and prevent plaque buildup around the affected area.
6. Follow-Up and Monitoring
- Regular Check-Ups: Ongoing evaluation by a dentist to monitor the condition and ensure resolution of symptoms.
Summary
Treatment for pericoronitis involves cleaning and debridement of the affected area, antibiotic therapy for infection, pain management, and, if necessary, surgical intervention such as operculectomy or tooth extraction. Maintaining good oral hygiene and follow-up care are also important for managing and preventing pericoronitis.
Leave a Reply
You must be logged in to post a comment.