What are the symptoms of a periapical abscess?
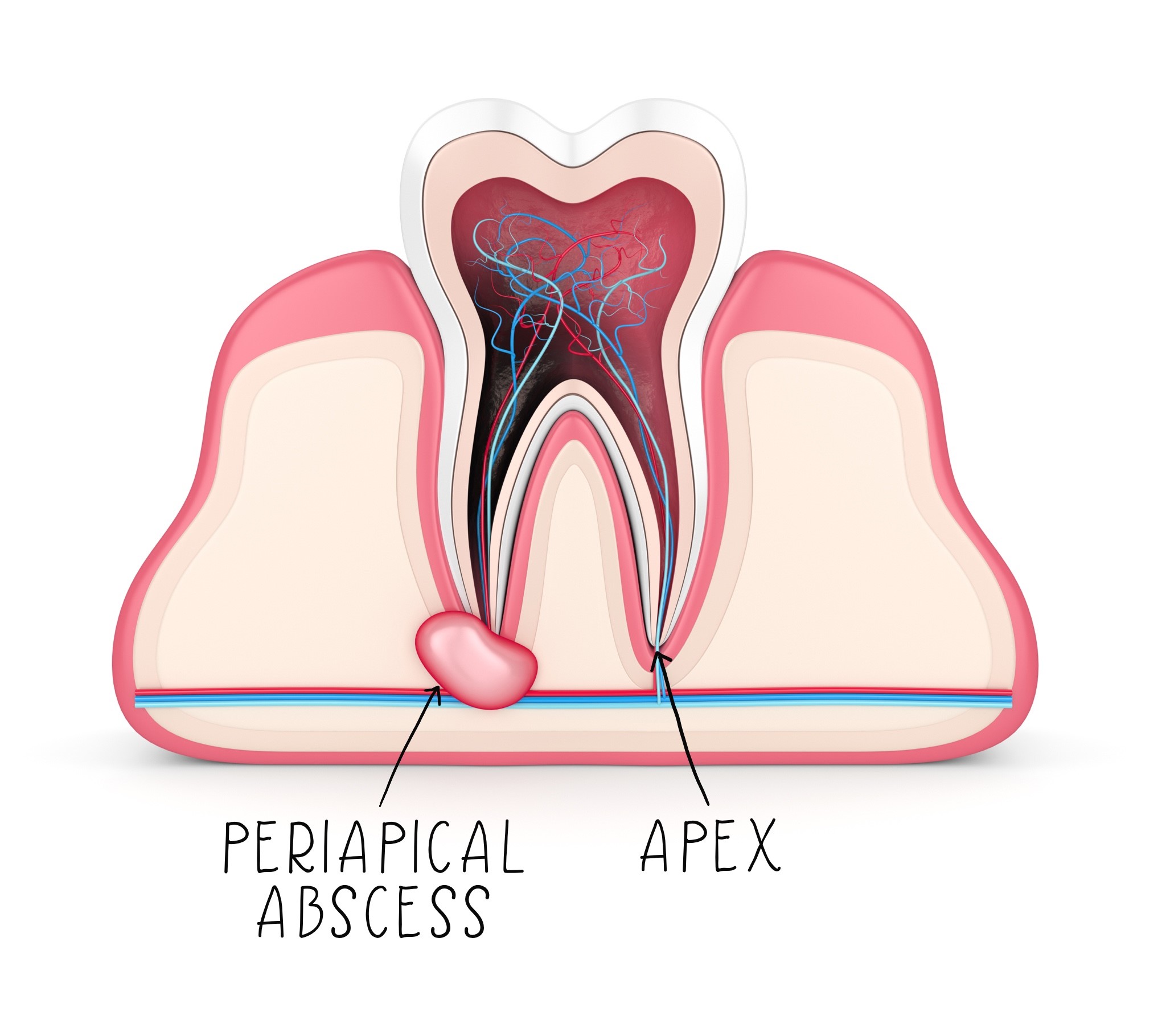
A periapical abscess is an infection that occurs at the tip of the root of a tooth, typically due to untreated dental caries (cavities) or trauma. It can cause a range of symptoms, including:
1. Tooth Pain
- Localized Pain: Persistent, throbbing pain around the affected tooth.
- Sensitivity: Increased sensitivity to hot or cold foods and drinks, or to pressure, such as when chewing.
2. Swelling
- Gum Swelling: Swelling of the gums near the affected tooth.
- Facial Swelling: In severe cases, swelling can extend to the face or neck.
3. Redness and Warmth
- Inflammation: The area around the tooth may appear red and feel warm to the touch due to inflammation.
4. Abscess Formation
- Pus Pocket: A visible lump or pimple-like swelling on the gum that may ooze pus.
5. Fever
- Systemic Symptoms: Elevated body temperature or fever as the body responds to the infection.
6. Bad Breath
- Foul Odor: An unpleasant odor in the mouth, often due to the infection and pus.
7. Difficulty Swallowing
- Swallowing Problems: Difficulty swallowing or a sore throat if the infection spreads.
8. Tooth Discoloration
- Tooth Changes: The affected tooth may appear darker or discolored.
9. General Malaise
- Feeling Unwell: General feeling of being unwell or fatigued due to the infection.
Summary
Symptoms of a periapical abscess include localized tooth pain, sensitivity, swelling of the gums and potentially the face, redness and warmth in the affected area, pus formation, fever, bad breath, difficulty swallowing, and general malaise. Prompt dental evaluation and treatment are important to manage the infection and prevent complications.
What are the causes of a periapical abscess?
A periapical abscess is caused by an infection at the tip of a tooth’s root, typically resulting from issues related to the tooth’s pulp or surrounding tissues. The main causes include:
1. Dental Caries (Cavities)
- Decay: Deep dental caries can reach the tooth’s pulp, leading to bacterial infection and abscess formation if left untreated.
2. Trauma
- Injury: Physical trauma to the tooth, such as a blow or fall, can damage the tooth’s pulp and lead to an abscess.
3. Tooth Fractures
- Cracks or Breaks: A fractured or cracked tooth can expose the pulp to bacteria, causing an infection and subsequent abscess.
4. Untreated Dental Infection
- Infection Spread: An untreated or poorly managed infection in the tooth or gums can spread to the root tip, forming an abscess.
5. Poor Dental Hygiene
- Inadequate Care: Neglecting oral hygiene can lead to plaque buildup, which contributes to tooth decay and increases the risk of infections.
6. Previous Dental Work
- Faulty Procedures: Incomplete or unsuccessful root canal treatments, or issues with dental fillings or crowns, can result in infection and abscess formation.
7. Gum Disease
- Periodontal Disease: Severe gum disease (periodontitis) can cause infection that may spread to the tooth’s root and lead to an abscess.
8. Root Canal Failure
- Treatment Issues: Failure of a previous root canal treatment to fully remove bacteria and seal the tooth can result in a periapical abscess.
9. Bacterial Infection
- Pathogenic Bacteria: Bacteria entering the pulp chamber through decay or trauma can proliferate, leading to an infection and abscess at the root tip.
10. Systemic Conditions
- Underlying Health Issues: Certain systemic health conditions that affect the immune system may increase the risk of infections, including periapical abscesses.
Summary
A periapical abscess is primarily caused by tooth decay, trauma, fractures, untreated infections, poor dental hygiene, issues with previous dental work, gum disease, and failures in root canal treatments. Proper dental care and prompt treatment of dental issues can help prevent the development of a periapical abscess.
How is the diagnosis of a periapical abscess made?
Diagnosing a periapical abscess involves a combination of clinical examination, imaging studies, and sometimes additional tests. Here’s a detailed approach to how the diagnosis is made:
1. Medical History
- Symptom Inquiry: Asking about symptoms such as tooth pain, swelling, sensitivity to hot or cold, fever, and bad breath.
- Dental History: Reviewing any history of dental issues, trauma, previous treatments, or recent dental work.
2. Clinical Examination
- Visual Inspection: Examining the affected tooth and surrounding area for signs of swelling, redness, and pus formation.
- Palpation: Gently pressing on the area around the tooth and gums to assess tenderness, swelling, and any fluctuation (indicating pus).
3. Tooth Testing
- Percussion Test: Gently tapping on the affected tooth to check for pain or sensitivity, which can indicate pulp involvement.
- Thermal Sensitivity Test: Applying hot or cold stimuli to the tooth to assess its response. Reduced sensitivity or prolonged pain may suggest pulp damage.
4. Radiographic Imaging
- X-rays:
- Periapical X-ray: The primary diagnostic tool for a periapical abscess. It shows the root and surrounding bone structure, revealing signs of bone loss or abscess formation at the root tip.
- Cone Beam Computed Tomography (CBCT): In complex cases or when additional detail is needed, a 3D scan may provide more information about the abscess and its extent.
5. Laboratory Tests
- Blood Tests: May be performed if there are systemic symptoms, such as fever, to check for signs of infection or other underlying health issues.
- Pus Culture: If there is drainage of pus, a culture may be done to identify the bacteria and guide antibiotic treatment.
6. Additional Diagnostic Procedures
- Vital Pulp Testing: In cases where the diagnosis is unclear, pulp vitality tests (such as electric pulp testing) may be used to determine if the tooth’s pulp is alive or necrotic.
Summary
The diagnosis of a periapical abscess is primarily based on clinical examination and radiographic imaging. X-rays are crucial for identifying the abscess and assessing its impact on the bone and surrounding tissues. Additional tests, such as blood tests and pus cultures, may be used to further evaluate the infection and guide treatment. Accurate diagnosis is essential for effective management and treatment of the abscess.
What is the treatment for a periapical abscess?
The treatment for a periapical abscess typically involves addressing both the infection and the underlying cause of the abscess. Here’s a comprehensive approach to managing a periapical abscess:
1. Drainage of the Abscess
- Incision and Drainage (I&D): The primary treatment is to drain the abscess. This involves making a small incision in the gum to release the pus and relieve pressure. This procedure is usually done under local anesthesia.
2. Root Canal Treatment
- Root Canal Therapy: If the tooth is salvageable, root canal treatment is often necessary. This involves removing the infected pulp from the tooth’s interior, cleaning and disinfecting the root canals, and sealing them with a material. This helps to eliminate the source of infection and prevent future abscesses.
3. Antibiotic Therapy
- Antibiotics: Prescribed to control and eradicate the bacterial infection. Common antibiotics include:
- Penicillin or amoxicillin: Often used for general bacterial infections.
- Clindamycin: May be prescribed if the patient is allergic to penicillin or if the infection is resistant to other antibiotics.
- Duration: The course typically lasts from 7 to 14 days, depending on the severity of the infection and the patient’s response.
4. Pain Management
- Pain Relievers: Over-the-counter medications such as ibuprofen or acetaminophen can help manage pain and reduce inflammation. In more severe cases, prescription pain medications may be necessary.
5. Warm Compresses and Sitz Baths
- Warm Compresses: Applying a warm compress to the affected area can help alleviate pain and promote drainage.
- Sitz Baths: Soaking the affected area in warm water can also help with comfort and hygiene.
6. Dental Restoration
- Restoration of the Tooth: After the infection is controlled and the root canal is complete, the tooth may need to be restored with a crown or filling to protect it and restore its function.
7. Follow-Up Care
- Regular Check-ups: Follow-up appointments are important to ensure that the infection has resolved and that the tooth is healing properly.
8. Management of Underlying Conditions
- Addressing Contributing Factors: If there are underlying issues contributing to the abscess, such as poor dental hygiene or existing gum disease, these need to be managed to prevent recurrence.
Summary
Treatment for a periapical abscess includes draining the abscess, performing root canal therapy if the tooth is viable, and using antibiotics to manage the infection. Pain management, warm compresses, and proper dental restoration are also essential. Follow-up care ensures the infection has resolved and helps prevent future issues.
Leave a Reply
You must be logged in to post a comment.