What are the symptoms of omphalocele?
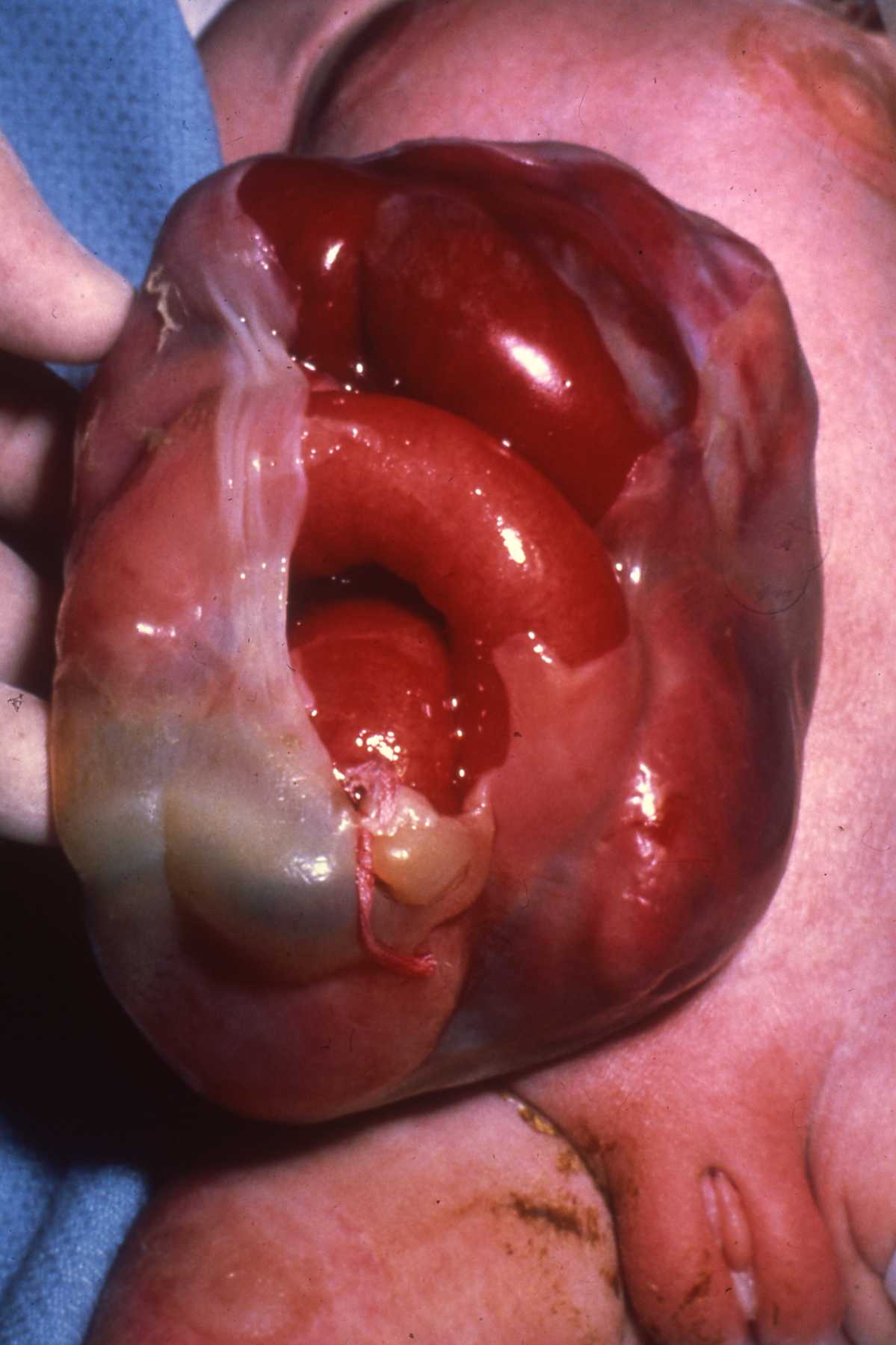
Omphalocele is a congenital condition in which the baby’s abdominal organs protrude through a defect in the abdominal wall at the base of the umbilical cord. The organs are typically covered by a thin membrane. Symptoms of omphalocele can vary depending on the size of the defect and the organs involved, but the following are common indicators:
Visible Signs
- Protrusion of Abdominal Organs:
- A noticeable bulge or sac at the base of the umbilical cord that contains organs like the intestines, liver, and sometimes other abdominal organs.
- The sac itself may be translucent or membranous.
Associated Symptoms
- Respiratory Distress:
- If the omphalocele is large, it may affect the development of the lungs, leading to breathing difficulties.
- Feeding Difficulties:
- Newborns may have trouble feeding due to the physical presence of the protruding organs or underlying gastrointestinal issues.
Associated Anomalies
- Other Congenital Anomalies:
- Omphalocele can be part of a broader syndrome (such as Beckwith-Wiedemann syndrome or others), and may be associated with other birth defects, such as:
- Heart defects
- Gastrointestinal malformations
- Changes in the development of other organs
Clinical Evaluation
- Diagnosis:
- Omphalocele is typically diagnosed during routine prenatal ultrasounds or soon after birth through physical examination.
- Additional Signs During Ultrasound:
- Imaging may show the presence of the abdominal contents within the sac outside of the abdominal cavity.
Conclusion
If omphalocele is suspected during pregnancy, further assessments may be carried out, and postnatal care will typically involve a multidisciplinary team for immediate management and surgical intervention. Prompt recognition and treatment are essential for improving outcomes for affected infants.
What are the causes of omphalocele?
Omphalocele is a congenital abdominal wall defect that occurs when an infant’s abdominal organs develop outside the body, protruding through the umbilical cord. The exact cause of omphalocele is not always known, but several factors are believed to contribute to its development:
1. Genetic Factors
- Chromosomal Abnormalities: Omphalocele is often associated with chromosomal anomalies such as trisomy 13 (Patau syndrome), trisomy 18 (Edwards syndrome), and Turner syndrome. These genetic conditions can disrupt normal development, leading to defects like omphalocele.
- Familial Patterns: There may be a genetic component, as omphalocele can sometimes occur in families, indicating a potential hereditary pattern.
2. Environmental Factors
- Maternal Factors: Certain maternal health conditions, such as diabetes or obesity, as well as exposure to certain medications, drugs, and environmental toxins during pregnancy, may increase the risk of omphalocele.
- Infections: Maternal infections, such as viral infections during pregnancy, may be linked to an increased risk of congenital malformations, including omphalocele.
3. Developmental Factors
- Failure of Abdominal Wall Closure: Omphalocele is thought to result from a failure of the embryonic abdominal wall to close properly by the end of the first trimester of pregnancy. This failure allows the abdominal organs to herniate through the umbilical ring.
4. Associated Malformations
- Omphalocele often occurs in the context of other birth defects. The presence of associated congenital anomalies can suggest a more complex developmental issue impacting multiple systems during fetal development.
5. Maternal Age
- Advanced maternal age (typically defined as 35 years or older) may be associated with a higher risk of chromosomal abnormalities and, consequently, birth defects like omphalocele.
Conclusion
While specific causes of omphalocele may not be identifiable in every case, it is recognized that a combination of genetic, environmental, and developmental factors likely play a role in its occurrence. Prenatal screening and genetic counseling may be advisable for families affected by omphalocele to understand the potential risks and implications for future pregnancies. If there are concerns about omphalocele or associated syndromes, consulting with a healthcare professional or a genetic counselor is recommended.
How is the diagnosis of omphalocele made?
The diagnosis of omphalocele can be made through various methods, primarily during pregnancy and shortly after birth. Here are the key steps and techniques used in diagnosing this condition:
Prenatal Diagnosis
- Ultrasound Imaging:
- Routine Ultrasound: Omphalocele is often identified during routine prenatal ultrasounds typically performed around 18-20 weeks of gestation. The ultrasound can reveal a bulge at the base of the umbilical cord, which may contain abdominal organs.
- Detailed Anatomy Scan: If an omphalocele is suspected, a more detailed scan may be performed to assess the extent of the defect, the organs involved, and to check for associated anomalies.
- Maternal Serum Screening:
- Although not a direct diagnostic tool for omphalocele, maternal serum alpha-fetoprotein (AFP) screening can indicate the presence of some fetal anomalies. Elevated levels of AFP may suggest a potential anomaly, prompting further investigation through ultrasound.
Postnatal Diagnosis
- Physical Examination:
- Upon birth, healthcare providers typically perform a physical examination of the newborn. The presence of an omphalocele can be diagnosed based on the observation of a sac-like structure at the base of the umbilical cord, containing abdominal contents.
- Imaging Studies:
- X-rays or CT Scans (after stabilization): In some cases, imaging may be used to assess the condition of the organs within the omphalocele, although these are typically reserved for after stabilization if further evaluation of associated anomalies is necessary.
Associated Evaluations
- Genetic Counseling and Testing:
- If omphalocele is diagnosed, especially in the context of other malformations, genetic counseling may be recommended. Chromosomal analysis (karyotyping) may be performed to check for associated genetic syndromes, especially if there are significant concerns about chromosomal abnormalities.
Summary
In summary, the diagnosis of omphalocele involves a combination of prenatal ultrasound imaging, maternal serum screening, and physical examination of the newborn after birth. Early diagnosis allows for careful planning and management of the infant’s care, addressing any associated anomalies and ensuring appropriate surgical intervention. If there are concerns related to omphalocele or its associated conditions, it is essential to consult with healthcare professionals specializing in pediatric care and genetics.
What is the treatment for omphalocele?
The treatment for omphalocele primarily involves surgical intervention to repair the defect and return the herniated organs to the abdominal cavity. The approach to treatment can vary based on the size of the omphalocele, the presence of associated congenital anomalies, and the overall health of the newborn. Here are the key treatment steps:
1. Initial Management
- Stabilization: Immediately after birth, the newborn is stabilized. This includes monitoring vital signs and ensuring the baby is breathing adequately. The omphalocele is often covered with a sterile, moist dressing to protect the exposed organs from injury and infection until surgical intervention can occur.
- Prevention of Hypothermia: Since exposed abdominal organs can lead to heat loss, appropriate measures are taken to maintain the infant’s body temperature.
2. Surgical Repair
- Primary Repair: If the omphalocele is small (contained) and the abdominal cavity can accommodate the herniated organs, a primary surgical repair can be performed shortly after stabilization. This involves closing the abdominal wall and placing the organs back inside the cavity.
- Stage Repair: For larger omphaloceles, where there is not enough space in the abdominal cavity to accommodate the herniated organs, a staged approach may be used. This may involve:
- Silo Placement: A plastic silo (a type of pouch) may be placed over the omphalocele to gradually allow the organs to return to the abdominal cavity over several days or weeks. As swelling reduces, the organs can be moved back inside, with final closure of the abdominal wall occurring later.
- Tissue Expansion: In some cases, tissue expanders may be used to increase the size of the abdominal wall while gradually allowing the organs to be accommodated.
3. Postoperative Care
- Monitoring: After surgery, the infant will be closely monitored for complications, such as infection, feeding difficulties, and abdominal compartment syndrome. Parental support and education are also essential during this time.
- Nutritional Support: Depending on the extent of surgery and any associated gastrointestinal issues, the baby may require nutritional support, including intravenous (IV) fluids or specialized feeding approaches (e.g., enteral feeding) until they are stable enough to feed normally.
4. Management of Associated Anomalies
- If there are other congenital abnormalities or syndromes associated with the omphalocele, additional interventions and specialist consultations may be necessary. The complete management plan would be tailored to address these needs.
5. Long-term Follow-up
- Regular follow-up with pediatric specialists, including surgeons and possibly geneticists, is crucial for monitoring growth and development, resolving any functional issues, and addressing any potential delayed complications.
Conclusion
The treatment of omphalocele requires a multidisciplinary approach that includes pediatric surgeons, neonatologists, and often other specialists, depending on the baby’s overall health and additional anomalies. Early diagnosis and timely surgical intervention are critical factors that significantly influence outcomes for infants with omphalocele.
Leave a Reply
You must be logged in to post a comment.