What are the symptoms of neurogenic bladder?
Neurogenic bladder refers to a dysfunction of the bladder caused by a neurologic condition that affects the nerves responsible for bladder control. This can result from various conditions, including spinal cord injuries, multiple sclerosis, Parkinson’s disease, stroke, and other neurological disorders. The symptoms of neurogenic bladder can vary widely depending on the underlying cause and the specific aspects of bladder function that are affected. Here are some common symptoms associated with neurogenic bladder:
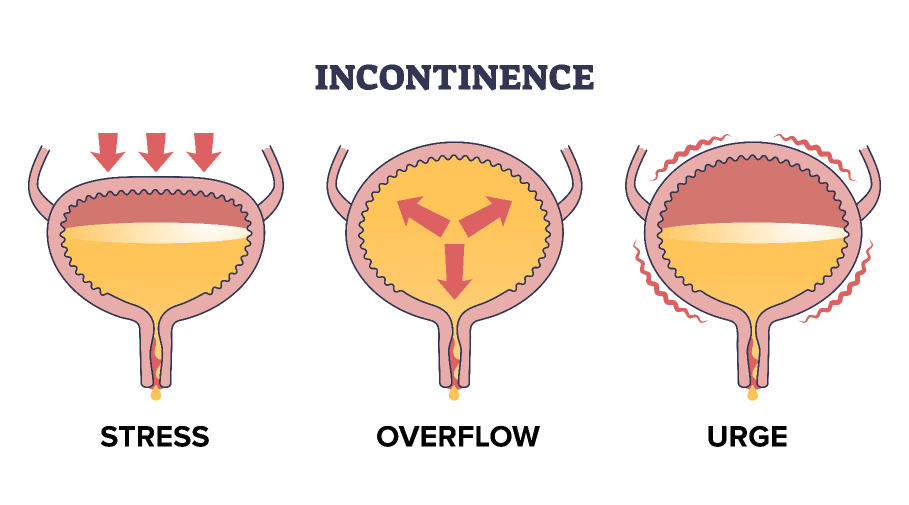
1. Incontinence:
- Urinary Incontinence: Inability to control urination, which may be characterized by:
- Overflow Incontinence: Frequent leakage of small amounts of urine due to an overly full bladder.
- Urge Incontinence: Sudden and intense urges to urinate that result in involuntary urine loss before reaching the toilet.
2. Retention:
- Urinary Retention: Difficulty in emptying the bladder completely which can lead to:
- Feeling of incomplete bladder emptying after urination.
- A constant urge to urinate or a feeling of pressure in the bladder area.
3. Frequent Urination:
- Increased Frequency: The need to urinate more often than usual, which may include nighttime urination (nocturia).
4. Urgency:
- Sudden or Strong Urges: A sudden and strong need to urinate that may lead to incontinence if not acted upon quickly.
5. Difficulty Starting Urination:
- Initiating Flow: Trouble starting the urine stream or a weak urine flow.
6. Abnormal Sensation:
- Change in Sensation: Reduced or abnormal sensations in the lower abdomen or genital area, which might affect the perception of bladder fullness.
7. Pain or Discomfort:
- Bladder Pain: Discomfort or pain in the bladder area, especially when it is full or during urination.
8. Recurrent Urinary Tract Infections (UTIs):
- Individuals with neurogenic bladder may be more susceptible to urinary tract infections as a result of improper bladder emptying or hygiene issues.
9. Kidney Problems:
- In chronic cases, due to untreated urinary retention or reflux of urine, individuals may develop complications such as hydronephrosis (swelling of a kidney due to urine buildup) or other kidney damage.
Conclusion:
The symptoms of neurogenic bladder can vary among individuals and may impact daily activities, quality of life, and overall health. If you or someone you know is experiencing symptoms suggestive of neurogenic bladder, it is essential to consult a healthcare provider for a thorough evaluation and proper management. Treatment options may include lifestyle modifications, medications, or interventions to improve bladder function and manage symptoms effectively.
What are the causes of neurogenic bladder?
Neurogenic bladder is caused by dysfunction of the bladder due to neurological conditions that affect the nerves controlling bladder function. The key causes of neurogenic bladder can be categorized based on the underlying neurological issues. Here are some of the most common causes:
1. Spinal Cord Injuries:
- Traumatic Injuries: Damage to the spinal cord from accidents, falls, or sports injuries can disrupt the nerves that communicate signals between the bladder and the brain, leading to neurogenic bladder.
- Complete or Incomplete Injury: Both complete and incomplete injuries can result in varying degrees of bladder dysfunction, often depending on the level and severity of the injury.
2. Neurological Disorders:
- Multiple Sclerosis (MS): MS can lead to nerve damage, affecting bladder control and function due to disrupted signals between the brain and the bladder.
- Parkinson’s Disease: This progressive neurological disorder can impact the control of the bladder, leading to symptoms such as urgency, frequency, and incontinence.
- Spina Bifida: A congenital condition where the spinal cord doesn’t close properly, leading to nerve damage that can affect bladder control.
- Stroke: A stroke can impair the brain’s ability to control bladder function, potentially leading to incontinence or retention.
- Alzheimer’s Disease and Dementia: Cognitive impairments can affect the ability to recognize the need to urinate, leading to incontinence.
3. Peripheral Nerve Disorders:
- Diabetic Neuropathy: Diabetes can cause nerve damage that impacts bladder control.
- Guillain-Barré Syndrome: An autoimmune disorder that can affect the peripheral nervous system, possibly leading to bladder dysfunction.
4. Surgical Procedures:
- Pelvic or Spinal Surgery: Operations affecting the pelvic area or spine may inadvertently damage nerves responsible for bladder control.
5. Congenital Disorders:
- Congenital Anomalies: Certain birth defects can affect the urinary system or the neurological control of the bladder.
6. Other Medical Conditions:
- Infections or Inflammation: Conditions that cause inflammation of the nervous system, such as meningitis or encephalitis, can lead to neurogenic bladder.
- Tumors: Tumors in the brain or spinal cord can damage local nerves that control bladder function.
Conclusion:
Neurogenic bladder can arise from a variety of conditions that affect the nervous system, impacting the communication between the bladder and the brain. Proper diagnosis of the underlying cause is crucial for effective treatment and management. If neurogenic bladder is suspected due to symptoms, it is important to consult a healthcare professional for evaluation, which may include neurological assessments, imaging studies, and urodynamic testing to understand the condition and develop an appropriate management plan.
How is the diagnosis of neurogenic bladder made?
The diagnosis of neurogenic bladder involves a comprehensive evaluation that includes a detailed medical history, physical examination, and a variety of diagnostic tests. The approach is designed to assess bladder function, underlying neurological issues, and to identify the causative factors. Here is an overview of the diagnostic process:
1. Medical History:
- Patient History: A healthcare provider will take a detailed history of the patient’s symptoms, including:
- Urination habits (frequency, urgency, volume, nighttime urination).
- Any incidents of incontinence or urinary retention.
- Associated symptoms such as pain, discomfort, or changes in sensation.
- Personal or family history of neurological disorders.
- Medical History: Documentation of any neurological conditions, surgeries, injuries, or medications that might affect bladder function.
2. Physical Examination:
- A physical examination may include:
- Neurological Assessment: Testing reflexes, sensation, and motor function to assess for any underlying neurological issues.
- Abdominal Examination: Checking for bladder distension and signs of urinary retention.
3. Urodynamic Studies:
- Urodynamics are a series of tests that evaluate how well the bladder and urethra store and release urine. They may include:
- Cystometry: Measures the pressure and volume of the bladder while it fills and assesses the bladder’s capacity and compliance.
- Urethral Pressure Profile: Assesses the pressure in the urethra to evaluate sphincter function.
- Post-Void Residual Measurement: A test performed after urination to determine if there is residual urine left in the bladder, indicating incomplete bladder emptying.
4. Imaging Studies:
- Ultrasound: An abdominal ultrasound can evaluate the volume of urine left in the bladder after urination and assess for any obstructions.
- MRI or CT Scans: Imaging can be used to visualize structural abnormalities in the spine or brain that may affect bladder function, such as tumors or spinal cord injuries.
5. Urinalysis:
- A urinalysis helps to rule out urinary tract infections (UTIs) or other abnormalities that might contribute to bladder symptoms.
6. Neurological Evaluation:
- Referral to a neurologist may be necessary for further assessment if a neurological cause is suspected, which could involve additional tests such as:
- Electromyography (EMG) or nerve conduction studies to assess nerve function.
- MRI of the brain or spinal cord to identify lesions or structural issues affecting nerve pathways.
7. Bladder Diary:
- Keeping a diary of fluid intake, urination habits, and symptoms over a specified period can help the healthcare provider understand the pattern of the bladder dysfunction.
Conclusion:
The diagnosis of neurogenic bladder requires a multifaceted approach to determine the underlying cause and assess bladder function. It is essential for effective management and treatment. If you or someone you know is experiencing symptoms of neurogenic bladder, consulting a healthcare professional, such as a urologist or neurologist, is crucial for obtaining a proper diagnosis and treatment plan tailored to the individual’s needs. Early diagnosis and intervention can significantly improve quality of life and bladder function.
What is the treatment for neurogenic bladder?
The treatment for neurogenic bladder is tailored to the underlying cause, the specific symptoms the patient is experiencing, and the overall impact on quality of life. The primary goals of treatment are to improve bladder function, prevent complications (such as urinary tract infections), and manage symptoms effectively. Treatment options may include:
1. Medications:
- Anticholinergic Agents: These medications can help reduce bladder spasms and increase bladder capacity. They are often used in cases of overactive bladder.
- Beta-3 Agonists: Medications such as mirabegron can help relax the bladder muscle and increase storage capacity.
- Alpha-Blockers: These can help relax the bladder neck and facilitate urinary flow, particularly in cases of urinary retention.
- Botulinum Toxin Injections: Botox can be injected into the bladder muscle to reduce involuntary contractions in cases of overactive bladder.
2. Catherization:
- Intermittent Catheterization: This involves the regular use of a catheter to empty the bladder at scheduled intervals. It is often recommended for patients with urinary retention to ensure complete bladder emptying and prevent complications.
- Indwelling Catheterization: In some cases, a Foley catheter may be used for continuous drainage, although it is usually a temporary solution due to the risk of infections.
3. Bladder Training:
- Bladder Training Programs: These programs may help train the bladder to hold larger volumes and reduce urinary urgency by gradually increasing the time between voiding.
- Scheduled Voiding: Establishing a regular schedule for urination can assist in managing symptoms and reducing incontinence.
4. Surgical Interventions:
- Surgery for Urinary Retention: Procedures to create a conduit for urine flow, such as bladder augmentation (increasing the bladder’s capacity) or bladder reconstruction, may be considered in complex cases.
- Sphincter Surgery: Surgical procedures may be performed to help improve urinary control, such as placement of an artificial urinary sphincter in cases of incontinence.
5. Neuromodulation Therapy:
- Sacral Neuromodulation: This procedure involves implanting a device that stimulates the nerves controlling the bladder, potentially improving bladder function and reducing symptoms.
6. Lifestyle Modifications:
- Diet Changes: Reducing irritants such as caffeine and alcohol can help manage symptoms.
- Fluid Management: Monitoring fluid intake can assist with both hydration and management of urinary frequency.
7. Physical Therapy:
- Pelvic Floor Exercises: Strengthening the pelvic floor muscles through exercises can improve bladder control and may alleviate some symptoms.
8. Psychosocial Support:
- Counseling or Support Groups: Emotional support and counseling can help individuals and families cope with the psychological aspects of living with neurogenic bladder.
Conclusion:
The management of neurogenic bladder typically involves a multidisciplinary approach, including urologists, neurologists, physical therapists, and other healthcare providers. Early diagnosis and personalized treatment planning are crucial for improving bladder function, preventing complications, and enhancing overall quality of life. If you suspect you have neurogenic bladder or experience relevant symptoms, seek advice from a healthcare professional for evaluation and a comprehensive treatment plan.
Leave a Reply
You must be logged in to post a comment.