What are the symptoms of a neural tube defect?
Neural tube defects (NTDs) are congenital malformations that occur when the neural tube, which forms the early spinal cord and brain, does not close properly during embryonic development. The severity of symptoms associated with neural tube defects can vary significantly depending on the type of defect and its location. The two most common types of neural tube defects are spina bifida and anencephaly. Here are the symptoms associated with these conditions:
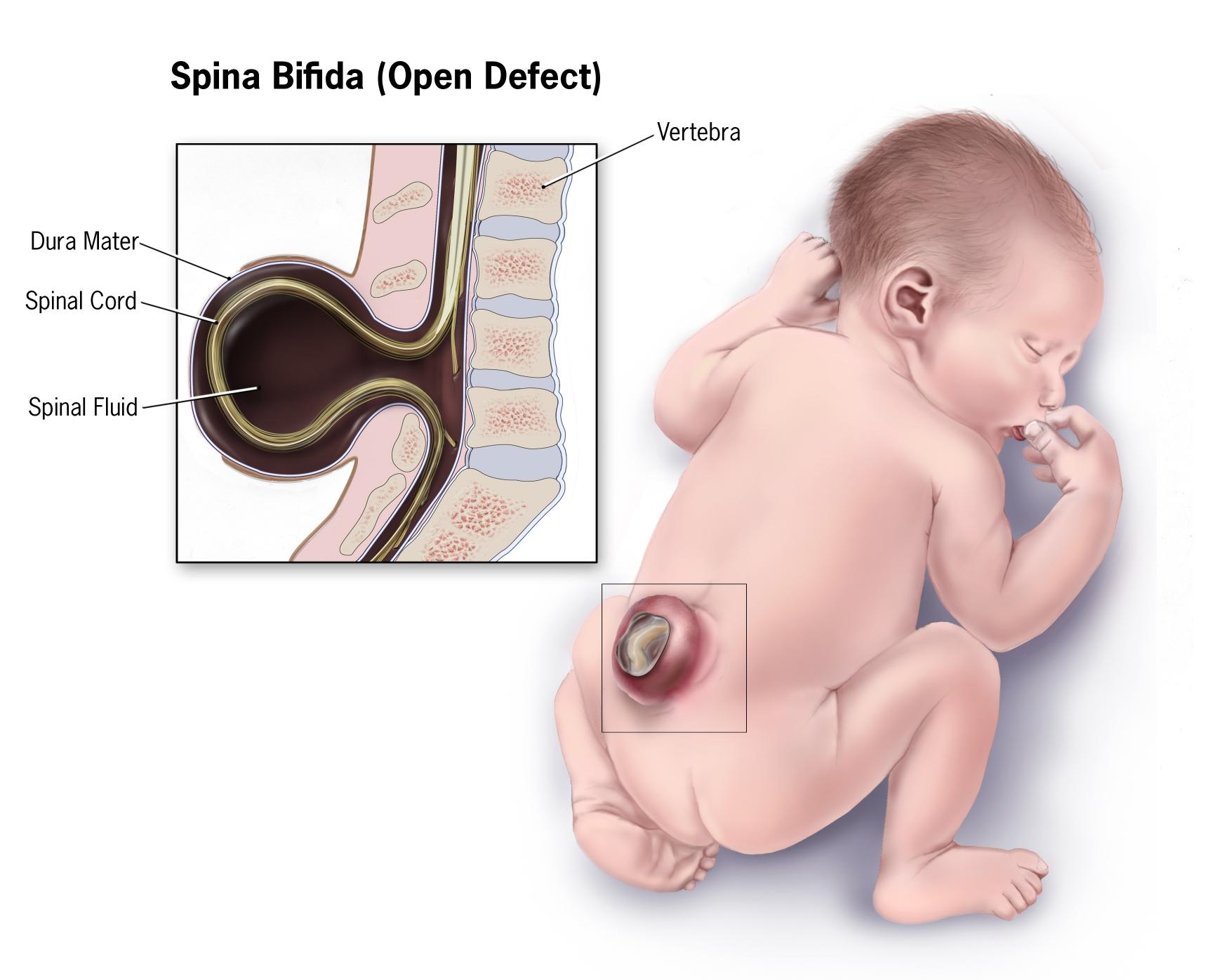
1. Spina Bifida:
Spina bifida occurs when the spinal column does not close completely, which can lead to varying degrees of impairment. Symptoms can range from mild to severe and may include:
- Physical Symptoms:
- Visible Defect: In cases like spina bifida occulta, there may be no external signs, but in more severe forms (such as spina bifida cystica), a sack-like structure filled with fluid may protrude from the back.
- Paralysis: Depending on the severity and location, individuals may experience partial or complete paralysis of the legs and lower body.
- Loss of Sensation: Individuals may have reduced sensation in the affected areas of the body.
- Neurological Symptoms:
- Hydrocephalus: Accumulation of cerebrospinal fluid in the brain, which can lead to increased intracranial pressure and requires monitoring and possibly treatment.
- Chiari Malformation: A condition where brain tissue extends into the spinal canal, leading to headaches and neurological issues.
- Bowel and Bladder Dysfunction:
- Incontinence or difficulty controlling bowel and bladder functions is common in spina bifida due to nerve damage.
- Orthopedic Problems:
- Deformities of the feet (clubfoot), hips, or spine may occur due to muscle imbalances and paralysis.
2. Anencephaly:
Anencephaly is a more severe form of neural tube defect where a significant portion of the brain and skull is absent. Symptoms associated with anencephaly include:
- Physical Symptoms:
- Absence of Forehead: Characteristic physical appearance with a flat or missing forehead.
- Malformed Skull: The skull may be poorly formed or absent in parts above the eyes, resulting in significant facial and cranial deformities.
- Neurological Symptoms:
- Complete Absence of Intact Brain: The brain may be severely underdeveloped, leading to a lack of brain function.
- Lack of Response: Infants with anencephaly typically do not respond to stimuli and have very limited brain activity.
- Life Expectancy:
- Infants born with anencephaly usually do not survive long after birth, often living only a few hours or days due to the absence of essential brain structures necessary for life.
Conclusion:
The symptoms of neural tube defects vary widely based on the type and severity of the defect. Spina bifida may result in a range of physical and neurological symptoms, while anencephaly leads to severe developmental issues with a very limited life expectancy. Early diagnosis, often achieved through prenatal screening, offers opportunities for intervention, including counseling and care planning, to address the specific needs of affected individuals and families. If there is a concern about a neural tube defect, it is essential to consult healthcare professionals for assessment and guidance.
What are the causes of a neural tube defect?
Neural tube defects (NTDs) occur when the neural tube, which develops into the brain and spinal cord, does not close properly during early embryonic development. The exact causes of NTDs are multifactorial, involving a combination of genetic, environmental, and nutritional factors. Here are the main known causes and risk factors associated with neural tube defects:
1. Nutritional Deficiencies:
- Folic Acid Deficiency: One of the most significant and well-established risk factors for neural tube defects is inadequate maternal intake of folic acid (vitamin B9) during the periconceptional period (the month before conception and during early pregnancy). Folic acid is essential for proper cell division and the formation of the neural tube.
2. Genetic Factors:
- Family History: A family history of neural tube defects increases the risk that future pregnancies may also be affected. Genetic predisposition plays a role in the likelihood of developing NTDs.
- Specific Genetic Mutations: Certain genetic mutations or syndromes may increase the risk of NTDs, though the relationship is complex and still subject to research.
3. Environmental Factors:
- Maternal Obesity: Maternal obesity before and during pregnancy is associated with an increased risk of neural tube defects.
- Diabetes: Poorly controlled pre-existing diabetes (particularly type 1 diabetes) in pregnant women is a known risk factor for NTDs.
- Teratogens: Exposure to certain medications, chemicals, or substances during pregnancy can increase the risk of NTDs, including:
- Certain anti-seizure medications (e.g., valproate).
- Some medications used for treating acne (e.g., isotretinoin).
- Environmental toxins such as pesticides and herbicides, although the evidence may vary.
4. Maternal Health and Conditions:
- Infections: Some maternal infections in the first trimester, such as rubella or viral infections, may increase the risk of neural tube defects.
- Hydrocephalus: Conditions affecting the mother’s health, such as vitamin deficiencies or issues with folate metabolism, may also contribute.
5. Ethnic and Geographic Differences:
- Ethnicity: Studies have shown that certain ethnic groups may have higher rates of neural tube defects, with variations attributed to genetic and dietary factors. For example, some studies indicate that people of Hispanic descent may have higher rates of NTDs compared to other populations.
6. Other Factors:
- Multiple Pregnancies: Having multiple pregnancies (twins, triplets, etc.) can slightly increase the risk.
- Age of the Mother: Young mothers (under 18) and older mothers (over 35) may be at higher risk for NTDs in their children.
Conclusion:
Neural tube defects arise from a complex interplay of genetic, environmental, and nutritional factors. The relationship between maternal folic acid intake and the prevention of NTDs is particularly important, and it is widely recommended that women of childbearing age ensure adequate folic acid intake before and during pregnancy to reduce the risk of NTDs. If there is a family history of NTDs or other risk factors, consulting with a healthcare provider before conception can help address potential concerns.
How is the diagnosis of neural tube defect made?
The diagnosis of neural tube defects (NTDs) typically occurs through a combination of prenatal screening, imaging studies, and sometimes postnatal evaluation. Here are the main steps involved in diagnosing neural tube defects:
1. Prenatal Screening:
- Maternal Serum Alpha-Fetoprotein (MSAFP) Test:
- During the second trimester (usually between weeks 15 and 20), a blood test may be conducted to measure levels of alpha-fetoprotein (AFP), a protein produced by the fetus. Elevated levels of AFP can indicate the presence of an open neural tube defect, although it is not definitive and may require further investigation.
- Quad Screen:
- This test measures four markers in the mother’s blood, including AFP, human chorionic gonadotropin (hCG), estriol, and inhibin A. Abnormal results can indicate an increased risk of NTDs and may prompt further testing.
- Ultrasound:
- A detailed ultrasound examination, typically performed around 18-20 weeks of gestation, can help visualize the developing fetus and identify physical signs of neural tube defects. Ultrasound can help detect:
- Spina Bifida: Characteristic findings may include visualizing a defect in the spinal column or abnormalities in the structure of the spine.
- Anencephaly: Absence of a significant portion of the brain or skull may be evident during the ultrasound.
2. Advanced Imaging:
- Fetal MRI:
- In some cases where ultrasound findings are inconclusive or further clarification is needed, a fetal MRI may be conducted to provide more detailed images of the fetal brain and spine, helping to confirm the diagnosis and assess the extent of the defect.
3. Postnatal Diagnosis:
- Physical Examination:
- If a neural tube defect is not detected prenatally, it may be identified at birth through a physical examination. Signs may include:
- Visible Defects: For example, spina bifida may present as a visible opening in the skin along the spine.
- Neurological Symptoms: Signs of neural impairment or paralysis during the newborn’s examination.
- Imaging Studies:
- If a diagnosis is suspected at birth or shortly thereafter, further imaging studies, such as ultrasound, CT scans, or MRI, may be used to evaluate the extent of the defect and any associated complications.
Conclusion:
The diagnosis of neural tube defects involves a combination of prenatal screening tests, imaging studies, and physical examination both prenatally and postnatally. Early diagnosis through routine screenings, such as serum alpha-fetoprotein tests and detailed ultrasounds, allows for better planning and management for families and healthcare providers. If a defect is detected, a multidisciplinary team can provide comprehensive care and support.
What is the treatment for a neural tube defect?
The treatment for neural tube defects (NTDs) varies depending on the type and severity of the defect, as well as any associated complications. The two most common types of NTDs are spina bifida and anencephaly, with treatment approaches differing significantly between the two. Here’s an overview of the management and treatment options for each type of neural tube defect:
1. Spina Bifida:
Spina bifida is a condition where the spinal column does not close completely, leading to varying degrees of impairment. Treatment options include:
A. Prenatal Treatment:
- Fetal Surgery: For certain severe cases of spina bifida, fetal surgery to close the defect in utero may be considered. This approach has been shown to improve outcomes for the child, such as reduced need for shunt placement for hydrocephalus and improved motor function.
B. Postnatal Treatment:
- Surgical Repair: After birth, most infants with spina bifida will undergo surgical repair of the defect. Timing may depend on the severity of the defect and the overall health of the infant, but surgery is usually performed within the first few days of life.
C. Additional Treatments:
- Management of Hydrocephalus: Many children with spina bifida develop hydrocephalus (accumulation of cerebrospinal fluid in the brain). This may require the placement of a shunt to drain excess fluid and prevent increased intracranial pressure.
- Rehabilitation Services: Physical therapy, occupational therapy, and other rehabilitation services may be necessary to help the child develop motor skills and mobility.
- Bowel and Bladder Management: Many individuals with spina bifida have issues with bowel and bladder control. Management may include medications, catheterization, or surgical interventions to assist with these functions.
- Ongoing Monitoring: Lifelong follow-up with a multidisciplinary team (including pediatricians, neurologists, urologists, and orthopedic specialists) is often needed to address complications and support developmental needs.
2. Anencephaly:
Anencephaly is a lethal condition characterized by the absence of a major portion of the brain, skull, and scalp. The key points regarding treatment include:
A. Supportive Care:
- Palliative Care: There is currently no cure for anencephaly, and treatment is primarily palliative. This focuses on providing comfort to the infant and the family.
B. Family Support:
- Counseling and Support Services: Parents may receive emotional support, counseling, and assistance in making decisions regarding the care and management of the child, including end-of-life care if needed.
- Planning for Birth: Families may be assisted in terms of planning for the delivery and postnatal care, acknowledging the potential for a very short life span for infants with anencephaly.
Conclusion:
The approach to managing neural tube defects is highly individualized based on the specific type of defect and associated complications. For spina bifida, surgical and rehabilitative interventions can significantly affect quality of life and functional abilities, while anencephaly requires a focus on supportive and palliative care. Early diagnosis, through prenatal testing and imaging, allows families to make informed decisions about care and treatment options. A multidisciplinary team of healthcare providers typically collaborates to provide comprehensive care and support for affected individuals and their families.
Leave a Reply
You must be logged in to post a comment.