What are the symptoms of nasal polyps?
Nasal polyps are soft, painless, noncancerous growths that can develop on the lining of the nasal passages or sinuses. They are often associated with chronic inflammation due to conditions such as asthma, allergies, or chronic sinusitis. Here are the common symptoms associated with nasal polyps:
1. Nasal Congestion:
- A feeling of blockage or obstruction in the nasal passages, leading to difficulty breathing through the nose and a sensation of fullness.
2. Runny Nose:
- Persistent nasal discharge that may be clear, cloudy, or mucous in nature. This can accompany other nasal symptoms.
3. Postnasal Drip:
- A feeling of mucus dripping down the back of the throat, which can lead to throat irritation, cough, or a sore throat.
4. Decreased Sense of Smell or Taste:
- Reduced ability to smell (hyposmia) or taste due to blockage of the olfactory receptors in the nasal cavity.
5. Facial Pain or Pressure:
- Discomfort, pressure, or pain in the face, particularly around the cheeks, forehead, or eyes, which may occur if the sinuses are affected.
6. Headaches:
- Chronic headaches can arise from sinus pressure caused by nasal polyps.
7. Snoring or Sleep Apnea:
- Nasal obstruction may lead to disrupted sleep patterns, increasing the likelihood of snoring or conditions like sleep apnea.
8. Frequent Sinus Infections:
- Recurrent or chronic sinus infections may occur due to blockage of drainage pathways in the sinuses.
9. Ear Pain or Pressure:
- A feeling of fullness or pressure in the ears, which can occasionally lead to hearing problems.
Conclusion:
Many of these symptoms may overlap with other conditions affecting the nasal passages, such as allergic rhinitis or chronic sinusitis. If a person experiences persistent symptoms or significant changes in their nasal or sinus health, it is advisable to consult a healthcare provider, such as an ear, nose, and throat (ENT) specialist, for an evaluation. They can confirm the presence of nasal polyps through physical examination and potentially recommend imaging studies or treatment options as necessary. Early diagnosis and treatment can help alleviate symptoms and improve the quality of life.
What are the causes of nasal polyps?
Nasal polyps are benign (noncancerous) growths that develop in the lining of the nasal passages or sinuses due to chronic inflammation. While the exact cause of nasal polyps is not always clear, several factors can contribute to their formation. Here are some common causes and associated conditions:
1. Chronic Inflammation:
- Chronic Sinusitis: Prolonged inflammation of the sinus lining, often due to infections or allergies, is one of the primary factors leading to the development of nasal polyps.
- Allergic Rhinitis: Allergies can cause chronic inflammation in the nasal passages, increasing the risk of polyps.
2. Asthma:
- People with asthma, particularly those who have chronic sinusitis or nasal polyps, often experience more severe symptoms. The inflammation associated with asthma can contribute to polyp formation.
3. Allergies:
- Individuals with sensitivities to environmental allergens, such as pollen, dust mites, mold, or pet dander, are at a higher risk for developing nasal polyps due to the resulting chronic inflammation.
4. Cystic Fibrosis:
- This genetic disorder affects the lungs and digestive system and is associated with thick, sticky mucus production. People with cystic fibrosis often develop nasal polyps due to chronic inflammation in the airways.
5. Aspirin Sensitivity:
- Some individuals with asthma and nasal polyps may experience exacerbations of symptoms when taking aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). This condition is known as aspirin-exacerbated respiratory disease (AERD) or Samter’s triad.
6. Non-Allergic Rhinitis:
- Conditions that cause inflammation of the nasal lining without an allergy component (such as hormonal changes, irritants, or infections) can also contribute to polyp development.
7. Genetic Factors:
- A family history of nasal polyps or related conditions can increase the risk, suggesting a possible hereditary component.
8. Other Chronic Conditions:
- Diseases like sarcoidosis or Churg-Strauss syndrome may also be associated with the development of nasal polyps due to chronic inflammation.
Conclusion:
While the exact pathophysiology of nasal polyps remains complex, chronic inflammation, allergic reactions, and underlying health conditions play significant roles in their development. If someone is experiencing symptoms associated with nasal polyps, such as nasal congestion, reduced sense of smell, or frequent sinus infections, it is important to consult a healthcare provider for proper evaluation, diagnosis, and treatment. Early intervention can help manage symptoms and improve quality of life.
How is the diagnosis of nasal polyps made?
The diagnosis of nasal polyps typically involves a comprehensive evaluation by a healthcare professional, often an ear, nose, and throat (ENT) specialist. The process generally includes several steps to identify the presence of nasal polyps and assess their characteristics. Here are the primary components involved in diagnosing nasal polyps:
1. Medical History:
- Symptom Assessment: The healthcare provider will inquire about the patient’s symptoms, including nasal congestion, persistent runny nose, loss of smell, facial pain or pressure, postnasal drip, and other related symptoms.
- Duration of Symptoms: Understanding how long the symptoms have been present and whether they are chronic or recurrent is important.
- Allergic History: The provider may ask about any history of allergies, asthma, or other respiratory conditions.
2. Physical Examination:
- Nasal Examination: A detailed physical examination of the nasal passages using an endoscope may be performed. This involves using a thin, flexible tube with a camera and light source that allows visualization of the nasal cavity and sinuses.
- Throat and Ear Examination: The provider may also check the throat and ears to rule out related issues or complications.
3. Imaging Studies:
- Computed Tomography (CT) Scan: If more information is needed, a CT scan of the sinuses may be ordered to provide detailed images of the nasal passages and sinuses. This can help identify the size, location, and extent of the polyps and other anatomical abnormalities. CT scans are particularly useful for evaluating chronic sinusitis and complex sinus pathology.
4. Allergy Testing:
- If allergies are suspected as a contributing factor, allergy testing (skin prick tests or blood tests) may be conducted to identify specific allergens that may be causing inflammation.
5. Biopsy (if necessary):
- In rare cases, a biopsy may be performed to rule out other conditions or to examine the tissue for atypical features. This is usually not necessary for diagnosing typical nasal polyps.
Conclusion:
The diagnosis of nasal polyps involves a thorough evaluation that includes a detailed history, physical examination, and possibly imaging studies. If you suspect you may have nasal polyps or are experiencing persistent nasal symptoms, it is important to consult a healthcare provider for a proper diagnosis and tailored treatment plan. Early diagnosis and management can help alleviate symptoms and improve overall quality of life.
What is the treatment for nasal polyps?
The treatment for nasal polyps aims to reduce their size, alleviate symptoms, and address any underlying conditions contributing to their formation. The approach can vary based on the severity of symptoms and the individual patient’s health status. Here are the primary treatment options for nasal polyps:
1. Medications:
- Nasal Corticosteroid Sprays:
- These are often the first line of treatment and are effective in reducing inflammation and the size of nasal polyps. Common options include fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort). Patients generally need to use these sprays regularly for the best results.
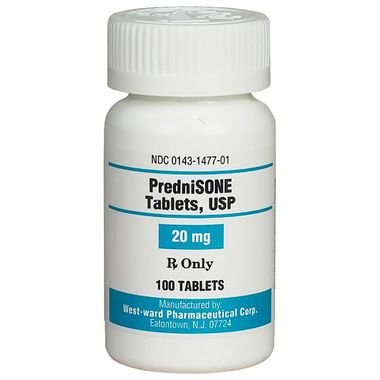
- Oral Corticosteroids:
- For more severe cases or when nasal corticosteroids are not effective, a short course of oral corticosteroids such as prednisone may be prescribed. This can quickly reduce inflammation and polyp size, but long-term use is typically avoided due to potential side effects.
- Saline Nasal Irrigation:
- Using saline sprays or rinses can help moisturize the nasal passages, clear out mucus, and improve symptoms.
- Antihistamines:
- If allergies are contributing to the inflammation, antihistamines (either oral or intranasal) may help alleviate symptoms.
- Biologics:
- For individuals with severe chronic rhinosinusitis with nasal polyps and poor response to corticosteroids, biologic medications (e.g., dupilumab, mepolizumab) may be considered. These target specific pathways in the inflammatory process.
2. Surgery:
- Endoscopic Sinus Surgery:
- If medications do not provide sufficient relief or if the polyps are large and causing significant obstruction, surgical intervention may be necessary. Endoscopic sinus surgery involves the removal of polyps and any obstructive tissue from the nasal passages and sinuses. This procedure is minimally invasive and usually performed under general or local anesthesia.
3. Managing Underlying Conditions:
- Control of Allergies or Asthma:
- Effective management of allergies or asthma may help prevent the recurrence of nasal polyps. This can include allergen avoidance strategies and appropriate medication.
4. Follow-Up Care:
- Monitoring and Maintenance: After treatment, regular follow-ups with a healthcare provider are important to monitor for recurrence. In some cases, long-term use of nasal corticosteroids may be recommended to maintain polyps at bay.
Conclusion:
The treatment of nasal polyps is individualized, based on symptoms and responses to initial therapies. If you suspect you have nasal polyps or are experiencing persistent nasal issues, it is advisable to consult a healthcare provider for an accurate diagnosis and comprehensive treatment plan. Early intervention can improve symptoms and enhance quality of life.
Leave a Reply
You must be logged in to post a comment.