What are the symptoms of a ventricular septal defect?
A ventricular septal defect (VSD) is a congenital heart defect where there is a hole in the wall (septum) that divides the lower chambers (ventricles) of the heart. The symptoms of a VSD can vary based on the size of the defect and the presence of other heart problems. Common symptoms include:
1. Heart Murmur:
- Unusual Sound: A characteristic “whooshing” sound may be heard through a stethoscope due to turbulent blood flow across the defect.
2. Shortness of Breath:
- Difficulty Breathing: Especially noticeable during physical activity or exertion, and may also occur at rest in severe cases.
3. Fatigue:
- Tiredness: Children with a VSD may tire easily, particularly during activities that involve physical exertion.
4. Rapid Breathing:
- Increased Breathing Rate: Breathing may become rapid or shallow, particularly in infants and young children.
5. Poor Feeding and Weight Gain:
- Feeding Difficulties: Infants with a VSD might struggle with feeding, leading to poor weight gain and growth.
6. Sweating:
- Excessive Sweating: Notably during feeding or activity, due to increased effort required to breathe or to cope with the heart defect.
7. Cyanosis:
- Bluish Skin or Lips: In severe cases, the skin, lips, or fingertips may take on a bluish color due to reduced oxygen levels in the blood (less common in VSD compared to other congenital heart defects).
8. Swelling:
- Edema: Swelling in the legs, ankles, or feet may occur, particularly if the defect leads to heart failure.
9. Recurrent Respiratory Infections:
- Frequent Infections: Increased risk of respiratory infections due to compromised heart function.
10. Heart Failure Symptoms:
- Signs of Heart Failure: In severe cases, symptoms such as fluid retention, weight gain, and difficulty in breathing may appear.
The severity of symptoms can depend on the size of the VSD and whether there is any associated heart condition. Small VSDs may cause few or no symptoms and might close on their own, while larger defects may require medical or surgical intervention to manage symptoms and prevent complications.
What are the causes of a ventricular septal defect?
A ventricular septal defect (VSD) is a congenital heart defect, meaning it is present at birth. The exact cause of VSDs is not always clear, but several factors may contribute to their development:
1. Genetic Factors:
- Inherited Conditions: VSDs can occur in families with a history of congenital heart defects. Genetic mutations or chromosomal abnormalities can play a role in the development of VSDs.
- Genetic Syndromes: Certain genetic syndromes, such as Down syndrome, DiGeorge syndrome, and other chromosomal disorders, are associated with an increased risk of VSD.
2. Environmental Factors:
- Maternal Health: Factors such as maternal diabetes, phenylketonuria (PKU), or certain infections during pregnancy can increase the risk of congenital heart defects, including VSD.
- Medications and Substance Use: The use of certain medications, drugs, or alcohol during pregnancy may contribute to the development of heart defects.
3. Maternal Age:
- Advanced Maternal Age: Older maternal age has been associated with a higher risk of congenital anomalies, including VSD.
4. Prenatal Exposure:
- Exposure to Toxins: Exposure to certain environmental toxins or infections during pregnancy may be linked to an increased risk of congenital heart defects.
5. Other Birth Defects:
- Associated Conditions: VSDs often occur alongside other congenital heart defects or birth defects, suggesting that some of the same factors contributing to those conditions may also cause VSD.
6. Idiopathic:
- Unknown Causes: In many cases, the exact cause of a VSD remains unknown, and the defect occurs sporadically without a clear underlying cause.
VSDs can vary widely in size and severity. Smaller defects may cause minimal symptoms or resolve on their own, while larger defects may require medical or surgical intervention. The interaction of genetic and environmental factors can influence the likelihood of developing a VSD.
What is the treatment for a ventricular septal defect?
The treatment for a ventricular septal defect (VSD) depends on the size of the defect, the symptoms it causes, and whether it is associated with other heart problems. Here’s an overview of the typical approaches to managing a VSD:
1. Observation and Monitoring:
- Small VSDs: Many small VSDs may close on their own over time and may not cause significant symptoms. Regular follow-up with a cardiologist is usually recommended to monitor the VSD and ensure it does not lead to complications.
2. Medications:
- Diuretics: To reduce fluid buildup and ease symptoms of heart failure if the VSD is causing significant problems.
- ACE Inhibitors: To help reduce blood pressure and decrease the workload on the heart, especially in cases with significant left-to-right shunting or heart failure.
- Antibiotics: Prophylactic antibiotics may be prescribed to prevent infections in some cases, particularly if there is a risk of infective endocarditis.
3. Lifestyle Modifications:
- Feeding and Growth Monitoring: In infants, ensuring proper feeding and monitoring growth to address any feeding difficulties or poor weight gain.
4. Surgical Intervention:
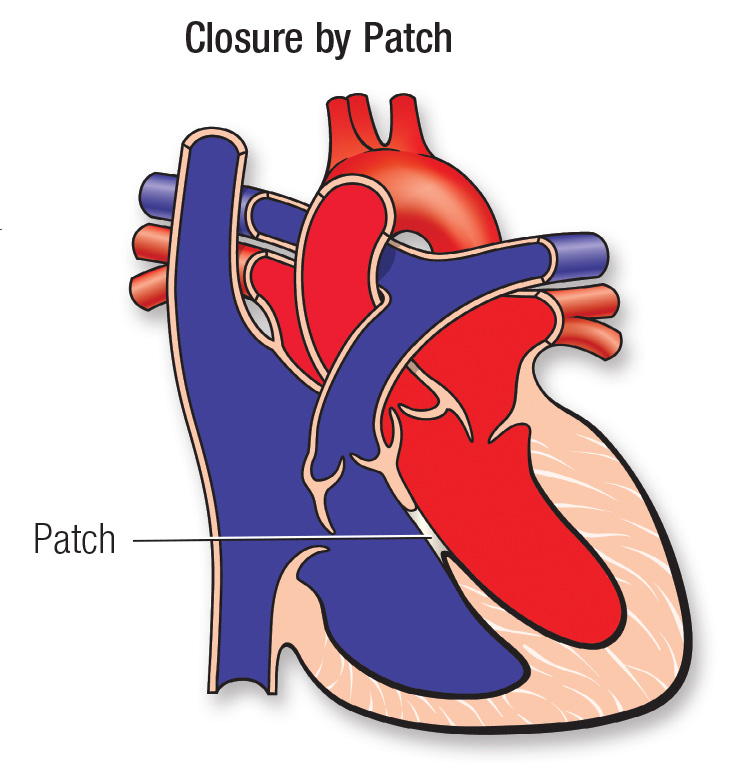
- VSD Closure Surgery: If the VSD is large, causing significant symptoms, or leading to complications such as heart failure, surgery may be recommended. The procedure involves closing the defect with a patch or using a device placed via a catheter-based approach (less invasive).
5. Catheter-Based Procedures:
- Device Closure: In some cases, a catheter-based procedure may be used to close the VSD with a specially designed device. This approach is less invasive than open-heart surgery and may be suitable for certain types of VSDs.
6. Treatment of Associated Conditions:
- Managing Other Heart Problems: If the VSD is associated with other congenital heart defects or conditions, these may also need to be addressed through medical or surgical means.
7. Follow-Up Care:
- Regular Check-Ups: Ongoing follow-up with a cardiologist to monitor the heart’s function, ensure proper growth and development, and detect any potential complications early.
The treatment plan for a VSD is individualized based on the specific characteristics of the defect and the overall health of the patient. In many cases, small VSDs may not require immediate treatment but rather careful monitoring. For larger or symptomatic VSDs, surgical or catheter-based interventions may be necessary to address the defect and improve heart function.
Leave a Reply
You must be logged in to post a comment.