What are the symptoms of a ventral hernia?
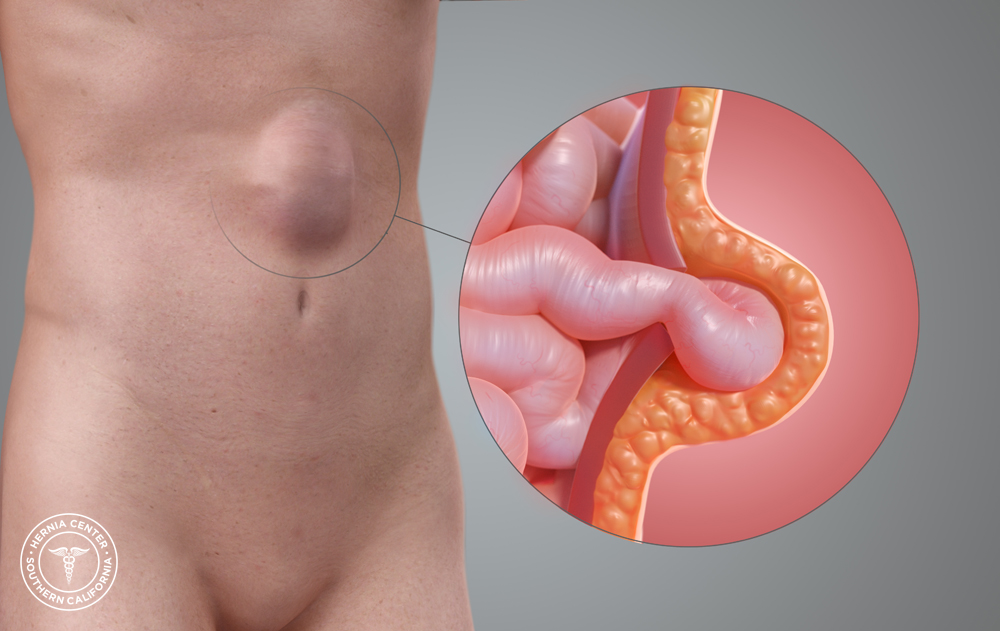
A ventral hernia occurs when tissue protrudes through a weak spot in the abdominal wall, often in the area of a previous surgical incision. The symptoms of a ventral hernia can include:
- Visible Bulge: A noticeable lump or bulge in the abdominal area, particularly in or around a previous surgical scar.
- Abdominal Pain: Discomfort or pain in the area of the hernia, which may worsen with physical activity, lifting, or straining.
- Pressure or Fullness: A feeling of pressure, heaviness, or fullness in the abdomen.
- Tenderness: The area around the hernia may be tender to the touch.
- Swelling: Swelling in the region of the hernia, which may become more prominent when standing or straining and may decrease or become less noticeable when lying down.
- Changes in Bulge: The bulge may increase in size with activities that put strain on the abdominal wall or decrease when at rest.
In some cases, a ventral hernia may become incarcerated or strangulated, leading to more severe symptoms such as:
- Severe Pain: Intense pain in the hernia area that may be persistent or worsening.
- Nausea and Vomiting: Symptoms of gastrointestinal distress if the hernia affects the bowel.
- Redness or Warmth: Signs of inflammation or infection in the hernia area.
- Inability to Reduce the Bulge: Difficulty pushing the bulge back into the abdomen or the bulge becoming fixed in place.
If you suspect you have a ventral hernia or experience any of these symptoms, it’s important to seek medical evaluation to determine the appropriate treatment and prevent potential complications.
What are the causes of a ventral hernia?
A ventral hernia is caused by a weakness in the abdominal wall, which allows tissue or organs to protrude through the weakened area. Common causes and contributing factors include:
1. Previous Abdominal Surgery:
- Incisional Hernia: A ventral hernia can occur at the site of a previous surgical incision. The incision weakens the abdominal wall, making it more susceptible to hernia formation.
2. Increased Abdominal Pressure:
- Heavy Lifting: Repeated heavy lifting or straining can increase pressure in the abdominal cavity, leading to a hernia.
- Chronic Coughing: Conditions that cause persistent coughing, such as chronic bronchitis, can contribute to increased abdominal pressure and hernia development.
- Constipation: Straining during bowel movements can contribute to the development of a hernia.
3. Obesity:
- Excess Weight: Increased body weight puts extra pressure on the abdominal wall, which can weaken it and lead to hernia formation.
4. Weakness in Abdominal Wall:
- Congenital Weakness: Some individuals may have a naturally weaker abdominal wall due to genetic factors or developmental issues.
- Aging: The abdominal wall can weaken with age, increasing the risk of hernias.
5. Pregnancy:
- Increased Abdominal Pressure: The growing uterus during pregnancy increases abdominal pressure, which can contribute to the development of a hernia.
6. Other Factors:
- Fluid Accumulation: Conditions that cause fluid accumulation in the abdomen, such as ascites, can increase abdominal pressure and contribute to hernia formation.
- Physical Activity: High-impact or strenuous activities, particularly if performed with improper technique, can strain the abdominal wall.
Addressing these risk factors through lifestyle modifications, proper technique in physical activities, and managing underlying conditions can help reduce the risk of developing a ventral hernia. If you have concerns about hernia risk or symptoms, consulting with a healthcare provider is recommended for evaluation and guidance.
What is the treatment for a ventral hernia?
The treatment for a ventral hernia typically involves both conservative measures and, in many cases, surgical intervention. The approach depends on the size, symptoms, and overall health of the patient. Here’s a general overview:
1. Conservative Management:
- Observation: For small, asymptomatic hernias, a healthcare provider may recommend monitoring the hernia without immediate intervention, especially if the hernia does not cause significant discomfort or complications.
- Lifestyle Modifications: Managing risk factors such as obesity, avoiding heavy lifting, and treating chronic cough or constipation can help prevent the hernia from worsening.
2. Surgical Treatment:
- Hernia Repair Surgery: The definitive treatment for a ventral hernia is usually surgical repair. This can be done through several techniques:
- Open Surgery: An incision is made in the abdominal wall, and the hernia is repaired by pushing the protruding tissue back into place and reinforcing the abdominal wall with sutures or a mesh patch.
- Laparoscopic Surgery: A minimally invasive technique where small incisions are made, and the hernia is repaired using special instruments and a camera. This method often results in less postoperative pain and a quicker recovery.
3. Postoperative Care:
- Wound Care: Proper care of the surgical site to prevent infection and promote healing.
- Pain Management: Medications to manage pain and discomfort following surgery.
- Gradual Return to Activity: Avoiding strenuous activities and heavy lifting as recommended by the healthcare provider to ensure proper healing.
4. Preventive Measures:
- Avoiding Strain: Taking precautions to avoid activities that increase abdominal pressure.
- Maintaining a Healthy Weight: Managing weight to reduce stress on the abdominal wall.
- Treating Underlying Conditions: Addressing issues such as chronic cough or constipation that can contribute to hernia development.
If you have a ventral hernia or are experiencing symptoms, consulting with a healthcare provider is essential to determine the best treatment plan based on your individual condition and health status.
Leave a Reply
You must be logged in to post a comment.