What are the symptoms of velopharyngeal insufficiency?
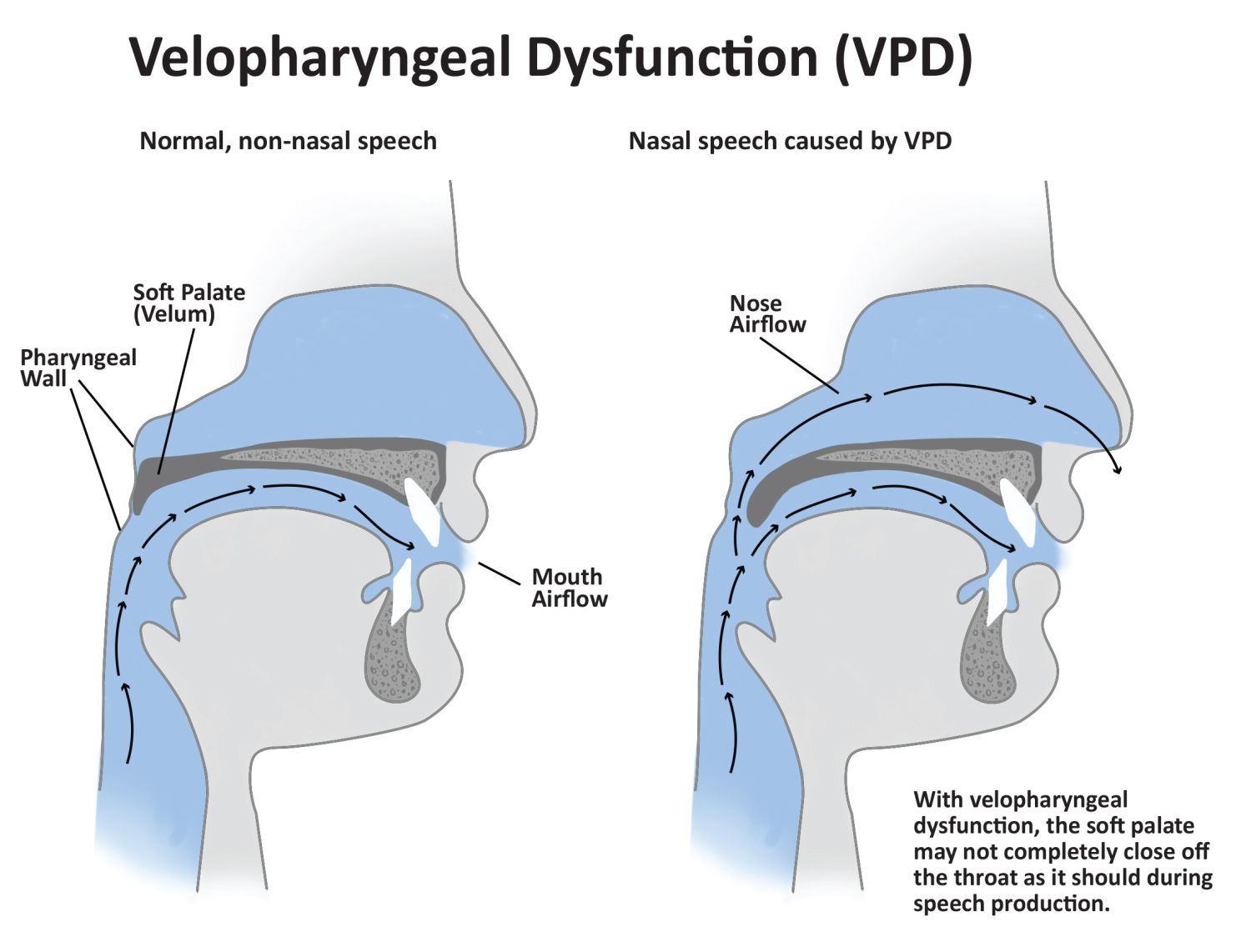
Velopharyngeal insufficiency (VPI) is a condition where there is inadequate closure of the velopharyngeal valve, which is responsible for separating the nasal cavity from the oral cavity during speech and swallowing. This insufficiency can lead to a range of symptoms, including:
Speech Symptoms:
- Nasal Speech: Speech may sound excessively nasal, often described as a “nasal” or “hypernasal” quality due to the leakage of air into the nasal cavity.
- Speech Difficulty: Difficulty in articulating certain sounds, particularly those that require proper oral closure, such as “p,” “b,” and “t.”
- Voice Changes: Reduced clarity in speech, with potential issues such as a weakened or muffled voice.
Feeding and Swallowing Symptoms:
- Nasal Regurgitation: Food or liquids may escape into the nasal cavity during swallowing, causing nasal regurgitation.
- Difficulty Swallowing: Trouble swallowing due to improper closure of the velopharyngeal valve, leading to aspiration (food or liquid entering the airway).
Physical Symptoms:
- Nasal Congestion: Chronic nasal congestion or recurrent ear infections may be associated with VPI due to improper airflow and pressure regulation.
- Gagging or Choking: Increased risk of gagging or choking while eating or drinking due to the difficulty in managing airflow and swallowing.
Other Considerations:
- Recurrent Ear Infections: VPI can sometimes lead to problems with the Eustachian tube function, contributing to frequent ear infections.
Symptoms of VPI can vary in severity and impact, depending on the degree of insufficiency and the presence of other related conditions. If VPI is suspected, a thorough evaluation by a speech-language pathologist and an ear, nose, and throat (ENT) specialist is usually recommended to assess the condition and determine appropriate management strategies.
What are the causes of velopharyngeal insufficiency?
Velopharyngeal insufficiency (VPI) can be caused by a variety of factors that impact the ability of the velopharyngeal valve to close properly during speech and swallowing. The primary causes include:
Structural Causes:
- Cleft Palate: A common cause of VPI, where there is a congenital gap in the roof of the mouth that affects the closure of the velopharyngeal valve.
- Submucous Cleft Palate: A type of cleft palate that is hidden beneath the mucous membrane, which can still lead to VPI despite not being visible on the surface.
- Velar Shortening: Abnormalities or shortening of the soft palate can prevent adequate closure.
Functional Causes:
- Neuromuscular Disorders: Conditions affecting the nerves or muscles involved in the movement of the soft palate, such as cerebral palsy or muscular dystrophy.
- Motor Speech Disorders: Conditions that impact the coordination of speech muscles, such as apraxia of speech, can lead to VPI.
Anatomical Abnormalities:
- Pharyngeal Wall Defects: Abnormalities in the pharyngeal wall or muscles that can hinder the proper closure of the velopharyngeal valve.
- Adenoid Hypoplasia: Underdevelopment of the adenoids, which can affect the closure of the velopharyngeal port.
Acquired Causes:
- Trauma or Surgery: Injury to the soft palate or pharynx due to trauma or surgical procedures can result in VPI.
- Post-Surgical Complications: Surgery related to the treatment of cleft palate or other conditions can sometimes result in insufficient closure of the velopharyngeal valve.
Genetic Conditions:
- Genetic Syndromes: Certain genetic conditions, such as 22q11.2 deletion syndrome (DiGeorge syndrome), can be associated with VPI due to related craniofacial anomalies.
Other Contributing Factors:
- Inflammation or Infection: Chronic inflammation or infection of the soft palate or pharynx can sometimes contribute to VPI.
The exact cause of VPI may vary depending on individual circumstances and may involve a combination of factors. Accurate diagnosis typically involves a comprehensive evaluation by specialists, including an ear, nose, and throat (ENT) physician and a speech-language pathologist, to determine the underlying cause and appropriate treatment.
What is the treatment for velopharyngeal insufficiency?
The treatment for velopharyngeal insufficiency (VPI) depends on the underlying cause, the severity of the insufficiency, and the specific symptoms experienced by the patient. Treatment options generally include a combination of surgical, therapeutic, and supportive interventions. Here’s an overview of common treatments:
Surgical Interventions:
- Palatoplasty: Surgical repair of the soft palate to correct structural issues and improve closure. This is often done in cases of cleft palate or velar abnormalities.
- Pharyngeal Flap Surgery: A surgical procedure that involves creating a flap of tissue from the back of the throat (pharynx) and attaching it to the soft palate to help improve closure.
- Sphincter Pharyngoplasty: A surgical procedure to create a new muscle sphincter around the velopharyngeal port to enhance closure.
Speech Therapy:
- Speech-Language Pathology: Therapy with a speech-language pathologist can help improve speech production by teaching techniques to manage and compensate for the insufficiency. This might include exercises to strengthen the soft palate muscles and strategies to reduce nasal air emission.
- Articulation Therapy: Focuses on improving the clarity of speech and the correct production of sounds affected by VPI.
Prosthetic Devices:
- Speech Prosthesis: In some cases, a prosthetic device, such as a palatal lift or obturator, may be used to help close the velopharyngeal port and improve speech.
Medical Management:
- Treatment of Underlying Conditions: If VPI is related to a specific medical condition or structural abnormality, addressing the underlying issue can help manage VPI. This may involve treating infections, managing neuromuscular disorders, or addressing other contributing factors.
Ongoing Monitoring and Follow-Up:
- Regular Assessments: Continuous follow-up with a team of specialists, including an ENT physician, speech-language pathologist, and possibly a craniofacial surgeon, to monitor progress and adjust treatment as needed.
Supportive Care:
- Nutritional Support: For individuals with feeding difficulties due to VPI, nutritional support and guidance may be necessary to ensure adequate intake and prevent complications.
Treatment plans are highly individualized and are often developed in collaboration with a multidisciplinary team. This team will assess the specific needs of the patient, including the severity of VPI and the presence of any related conditions, to determine the most appropriate interventions and strategies for management.
Leave a Reply
You must be logged in to post a comment.