What are the symptoms of vasodilation?
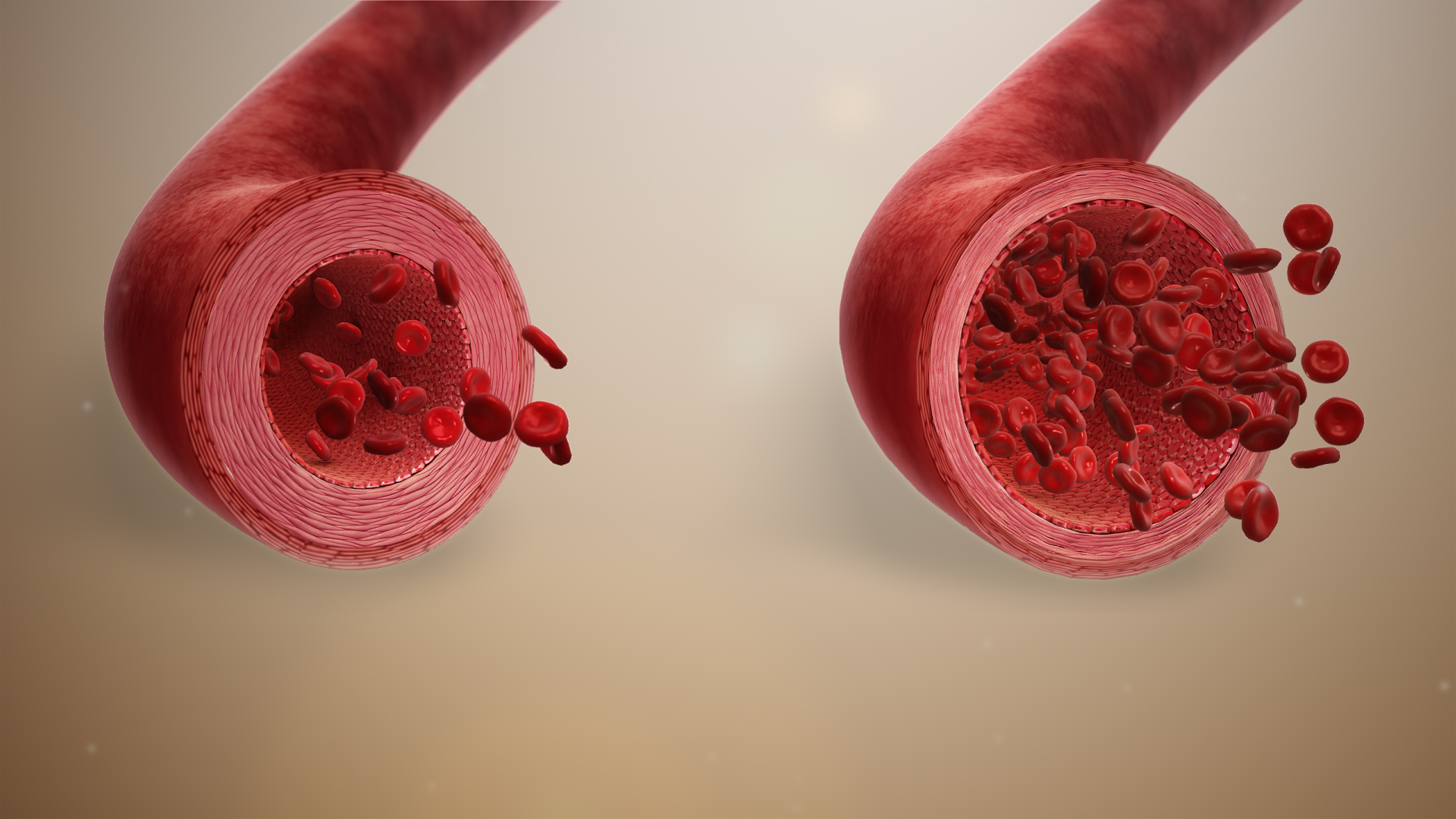
Vasodilation refers to the widening of blood vessels, which results in increased blood flow and reduced blood pressure. The symptoms of vasodilation can vary depending on the cause, the extent of the vasodilation, and the areas of the body affected. Common symptoms include:
General Symptoms:
- Flushed or Warm Skin: The skin may appear red or feel warm to the touch due to increased blood flow near the skin’s surface.
- Headache: The widening of blood vessels in the brain can lead to pressure changes that cause headaches.
- Dizziness or Lightheadedness: A sudden drop in blood pressure due to vasodilation can cause dizziness, especially when standing up quickly (orthostatic hypotension).
- Nausea: Changes in blood flow and pressure can sometimes lead to feelings of nausea.
- Fatigue or Weakness: A decrease in blood pressure can lead to feelings of fatigue, lethargy, or generalized weakness.
- Fainting (Syncope): If vasodilation leads to a significant drop in blood pressure, it can result in fainting.
Localized Symptoms:
- Swelling (Edema): In some cases, increased blood flow can cause fluid to accumulate in certain areas, leading to localized swelling.
- Nasal Congestion: Vasodilation in the nasal passages can cause a stuffy nose, commonly seen in conditions like allergic rhinitis.
Symptoms Associated with Specific Conditions:
- Heat Intolerance and Sweating: Vasodilation is a natural response to overheating. Excessive vasodilation in response to heat can lead to excessive sweating and difficulty tolerating warm environments.
- Migraine Symptoms: In some people, vasodilation in the brain is linked to migraines, leading to throbbing pain, sensitivity to light and sound, and visual disturbances.
While vasodilation is a normal and often beneficial physiological response, excessive or inappropriate vasodilation can cause discomfort and health issues, especially if it leads to dangerously low blood pressure.
What are the causes of vasodilation?
Vasodilation occurs when blood vessels widen due to the relaxation of the smooth muscle cells in the vessel walls. This process increases blood flow and lowers blood pressure. There are several causes of vasodilation, which can be categorized into physiological, environmental, and pathological factors:
Physiological Causes:
- Exercise: During physical activity, muscles require more oxygen, so blood vessels dilate to increase blood flow and supply oxygen and nutrients.
- Body Temperature Regulation: When the body is overheated, blood vessels near the skin surface dilate to release excess heat, helping to cool the body down.
- Hormonal Changes: Hormones like adrenaline, acetylcholine, and nitric oxide trigger vasodilation as part of various bodily processes.
- Inflammatory Response: Inflammation due to injury or infection can cause blood vessels to dilate to allow more immune cells to reach the affected area.
Environmental Causes:
- Heat Exposure: High environmental temperatures cause blood vessels to widen as the body tries to dissipate heat.
- Dietary Factors: Certain foods, such as those rich in nitrates (like beets and leafy greens), and spicy foods can cause vasodilation. Alcohol can also dilate blood vessels, leading to temporary flushing and warmth.
Pathological Causes:
- Allergic Reactions: During an allergic response, histamines are released, which cause vasodilation and contribute to symptoms like redness and swelling.
- Medications: Drugs like vasodilators (e.g., nitroglycerin), blood pressure medications, and even some antidepressants can cause vasodilation.
- Medical Conditions: Conditions like sepsis, anaphylaxis, and migraines involve abnormal or excessive vasodilation as part of their pathology.
Other Causes:
- Stress and Emotional Responses: Intense emotions, such as anger or embarrassment, can trigger the release of hormones that lead to vasodilation, causing skin flushing.
- Vasoactive Substances: Certain chemicals, including nitric oxide and prostaglandins, act directly on blood vessels to cause vasodilation.
Vasodilation is usually a normal and necessary bodily response. However, when excessive or uncontrolled, it can contribute to symptoms like low blood pressure, dizziness, and fainting.
What is the treatment for vasodilation?
The treatment for vasodilation depends on its underlying cause, the severity of symptoms, and any related health conditions. Here are common approaches to managing or treating vasodilation:
Lifestyle Modifications:
- Hydration: Ensuring adequate fluid intake can help maintain blood pressure and prevent symptoms associated with excessive vasodilation.
- Dietary Changes: Eating a balanced diet with a focus on foods that support healthy blood pressure can be beneficial. Avoiding excessive alcohol, which can cause vasodilation, may also help.
- Avoiding Triggers: If certain foods, beverages, or environmental factors (like extreme heat) are known to trigger symptoms, avoiding them can help manage vasodilation.
Medications:
- Vasoconstrictors: In cases where vasodilation causes significant symptoms like hypotension, medications that constrict blood vessels (such as midodrine) may be prescribed to counteract the effects.
- Fluid and Salt Supplements: In some cases, increasing fluid and salt intake under medical supervision can help maintain blood pressure and manage symptoms.
Medical Treatments:
- Compression Therapy: For localized vasodilation causing swelling, such as in the legs, compression stockings or devices may help manage symptoms by improving blood flow.
- Temperature Regulation: Using cooling or heating measures appropriately can help manage symptoms related to temperature-induced vasodilation. For instance, avoiding overheating or dressing appropriately for cold weather.
Treating Underlying Conditions:
- Managing Allergies: For allergic reactions causing vasodilation, antihistamines and other allergy medications can reduce symptoms.
- Treating Migraines: For migraines associated with vasodilation, medications specifically for migraine management, including triptans or preventative treatments, can be effective.
- Addressing Infections or Inflammations: Treating underlying infections or inflammatory conditions that lead to vasodilation can help alleviate symptoms.
Additional Measures:
- Elevating the Legs: In cases of orthostatic hypotension (low blood pressure upon standing), elevating the legs or using compression stockings can help improve blood flow and reduce dizziness.
- Behavioral Therapies: Techniques such as cognitive-behavioral therapy (CBT) or biofeedback may help manage symptoms related to stress-induced vasodilation.
Medical Consultation:
- Diagnosis and Management: For persistent or severe symptoms, consulting with a healthcare provider is crucial for accurate diagnosis and tailored treatment. They can perform tests to identify the underlying cause and recommend appropriate treatment strategies.
Effective management of vasodilation often involves addressing both the symptoms and the underlying causes to improve overall health and well-being.
Leave a Reply
You must be logged in to post a comment.