What are the symptoms of uterine prolapse?
Symptoms of uterine prolapse can vary depending on the severity of the condition. Common symptoms include:
- Pelvic pressure or heaviness: A sensation of heaviness or pressure in the pelvis is a common symptom.
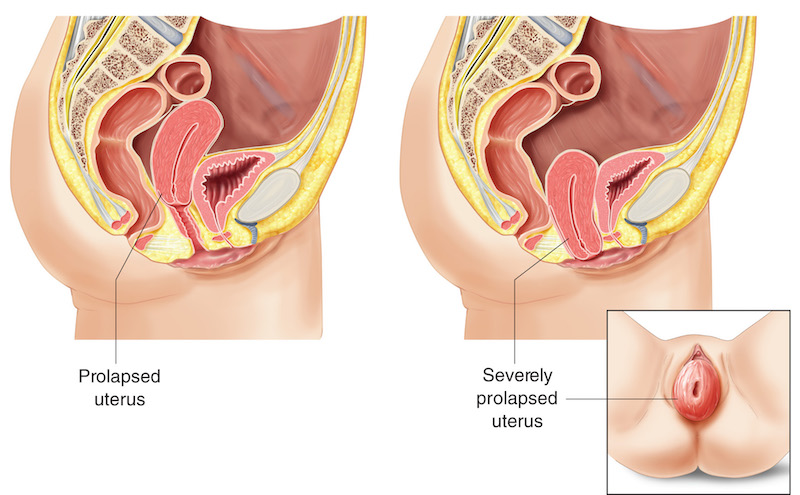
- Protrusion from the vagina: In more severe cases, part of the uterus may be felt or seen protruding from the vaginal opening.
- Vaginal fullness or bulging: A feeling of something “falling out” of the vagina.
- Lower back pain: Discomfort or pain in the lower back.
- Urinary issues: Problems such as urinary incontinence, difficulty starting to urinate, frequent urination, or a sensation of incomplete bladder emptying.
- Bowel problems: Constipation, difficulty with bowel movements, or a feeling of incomplete bowel evacuation.
- Sexual difficulties: Discomfort or pain during intercourse.
- Vaginal bleeding or discharge: Unusual bleeding or increased discharge may occur.
- Worsening symptoms with activity: Symptoms may worsen after prolonged standing, walking, or physical activity and may improve when lying down.
Uterine prolapse can range from mild to severe, with symptoms often worsening over time if left untreated.
What are the causes of uterine prolapse?
Uterine prolapse occurs when the pelvic floor muscles and ligaments weaken, allowing the uterus to slip down into or protrude out of the vagina. Common causes include:
- Childbirth trauma: Vaginal deliveries, especially of large babies or multiple deliveries, can strain and weaken pelvic muscles and ligaments, leading to prolapse.
- Aging and menopause: As estrogen levels decrease with age, tissues that support the pelvic organs can lose strength and elasticity.
- Obesity: Excess weight puts additional pressure on the pelvic floor, increasing the risk of prolapse.
- Chronic coughing: Persistent coughing from conditions like chronic bronchitis, asthma, or smoking can strain the pelvic floor muscles.
- Chronic constipation: Frequent straining during bowel movements can weaken the pelvic muscles over time.
- Hysterectomy: Removal of the uterus can sometimes lead to weakened support for the remaining pelvic organs.
- Heavy lifting: Regularly lifting heavy objects can strain the pelvic floor muscles.
- Genetics: Some women are genetically predisposed to having weaker connective tissues, making them more susceptible to prolapse.
Uterine prolapse is often a result of a combination of these factors, with age and childbirth being the most significant contributors.
What is the treatment for uterine prolapse?
Treatment options for uterine prolapse vary depending on the severity of the condition, the patient’s age, overall health, and treatment preferences. Options include:
Non-Surgical Treatments
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic muscles can help alleviate mild symptoms by improving support for the uterus.
- Vaginal Pessary: A silicone or rubber device is inserted into the vagina to support the uterus and prevent it from prolapsing further. This is a good option for women who are not candidates for surgery or prefer a non-surgical approach.
- Hormone Therapy: For postmenopausal women, estrogen therapy (vaginal or systemic) may help strengthen and improve the tone of pelvic tissues.
Surgical Treatments
- Hysterectomy: Removing the uterus can be an option for severe prolapse, especially for women who do not plan to have more children.
- Uterine Suspension (Uterosacral Ligament Suspension or Sacrohysteropexy): The uterus is repositioned and secured using ligaments or mesh, preserving the uterus while providing support.
- Vaginal Mesh Repair: Surgical mesh is used to support the pelvic organs. This procedure can be done transvaginally or through the abdomen. Note that mesh use is sometimes associated with complications.
Lifestyle Modifications
- Weight Management: Losing weight can reduce pressure on the pelvic floor.
- Avoid Heavy Lifting: Reducing strain on the pelvic muscles can help prevent further worsening of prolapse.
- Manage Chronic Conditions: Addressing chronic cough or constipation can prevent additional stress on the pelvic floor.
The choice of treatment depends on factors like symptom severity, desire to preserve fertility, and the patient’s overall health. Consultation with a gynecologist or urogynecologist is crucial for determining the best approach.
Leave a Reply
You must be logged in to post a comment.