What are the symptoms of a septate uterus?
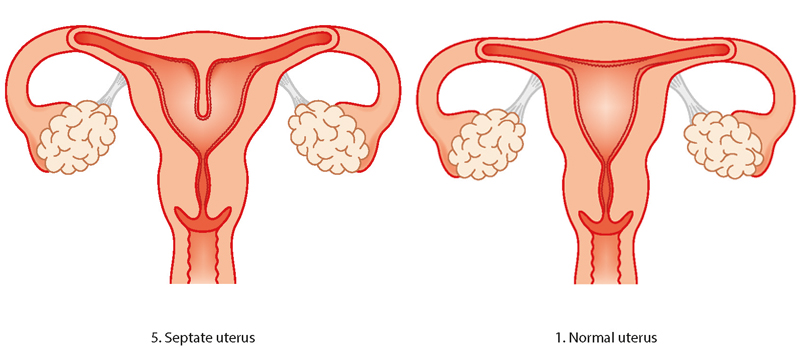
A septate uterus is a congenital uterine anomaly where a fibrous or muscular band of tissue, called a septum, divides the uterine cavity into two sections. This condition can vary in severity, and the symptoms can range from mild to significant, depending on the extent of the septum. Common symptoms associated with a septate uterus include:
- Recurrent Miscarriages: One of the most common symptoms is recurrent pregnancy loss. Women with a septate uterus are more likely to experience miscarriages, often in the first trimester.
- Infertility: Some women with a septate uterus may have difficulty conceiving. The septum can interfere with the implantation of an embryo or cause issues during early pregnancy.
- Preterm Labor: If pregnancy progresses, there is a higher risk of preterm labor or early delivery due to the abnormal shape of the uterus.
- Abnormal Menstrual Bleeding: Although less common, some women with a septate uterus may experience irregular or abnormal menstrual bleeding.
- Pain or Discomfort: Some women may experience pelvic pain or discomfort, particularly during menstruation or sexual intercourse, though this is not always the case.
- Asymptomatic: It’s important to note that many women with a septate uterus may not have any noticeable symptoms and may only discover the condition during imaging tests, such as an ultrasound or MRI, often when investigating fertility issues or recurrent miscarriages.
The symptoms and their severity can vary widely depending on the extent of the septum and how much it affects the uterine cavity.
What are the causes of a septate uterus?
A septate uterus is a congenital condition, meaning it occurs during fetal development and is present at birth. The condition results from abnormal development of the uterus during the early stages of pregnancy. Here’s how it happens:
- Fetal Development: During normal fetal development, the uterus begins as two separate structures called Müllerian ducts. These ducts typically fuse together to form a single, hollow uterine cavity. In the case of a septate uterus, the ducts fuse normally, but the tissue that separates them does not fully dissolve, leaving a septum (a band of tissue) that divides the uterine cavity into two sections.
- Genetic Factors: While the exact cause of a septate uterus is not well understood, it is believed to be related to genetic factors or disruptions in the normal developmental process. There may be a hereditary component, as uterine anomalies can sometimes run in families.
- Developmental Anomaly: The failure of the septum to fully resorb is simply a developmental anomaly. There are no known external factors during pregnancy, such as lifestyle or environmental influences, that cause this condition.
A septate uterus is one of several types of Müllerian duct anomalies, which are a group of congenital uterine abnormalities. It’s important to note that having a septate uterus is not typically associated with any specific cause or behavior during pregnancy; it is a naturally occurring condition that develops during fetal growth.
What is the treatment for a septate uterus?
The treatment for a septate uterus typically involves a surgical procedure called a hysteroscopic metroplasty or hysteroscopic resection. This procedure is designed to remove the septum and restore the normal shape of the uterine cavity. Here’s how the treatment works:
- Hysteroscopic Metroplasty: The most common and preferred treatment for a septate uterus is hysteroscopic metroplasty. This is a minimally invasive procedure where a surgeon uses a hysteroscope (a thin, lighted tube inserted through the vagina and cervix into the uterus) to visualize the septum. The surgeon then uses specialized surgical instruments to carefully cut and remove the septum, creating a single, unified uterine cavity.
- Outpatient Procedure: Hysteroscopic metroplasty is typically performed on an outpatient basis, meaning patients can go home the same day. The procedure is usually done under general anesthesia or local anesthesia with sedation.
- Recovery: Recovery from hysteroscopic metroplasty is generally quick. Most patients can return to normal activities within a few days. Some mild cramping or spotting may occur for a few days after the procedure.
- Follow-Up Care: After the procedure, follow-up care may include imaging studies, such as ultrasound or MRI, to ensure that the septum has been fully removed and that the uterine cavity is healing properly. In some cases, a temporary intrauterine device (IUD) may be placed to help prevent scar tissue formation during the healing process.
- Fertility Improvement: The removal of the septum can significantly improve fertility outcomes, reduce the risk of miscarriage, and lower the likelihood of complications during pregnancy.
In cases where the septum is minor or not causing significant issues, treatment may not be necessary. However, for women experiencing recurrent miscarriages, infertility, or other complications due to a septate uterus, hysteroscopic metroplasty is the standard and effective treatment option.
Leave a Reply
You must be logged in to post a comment.