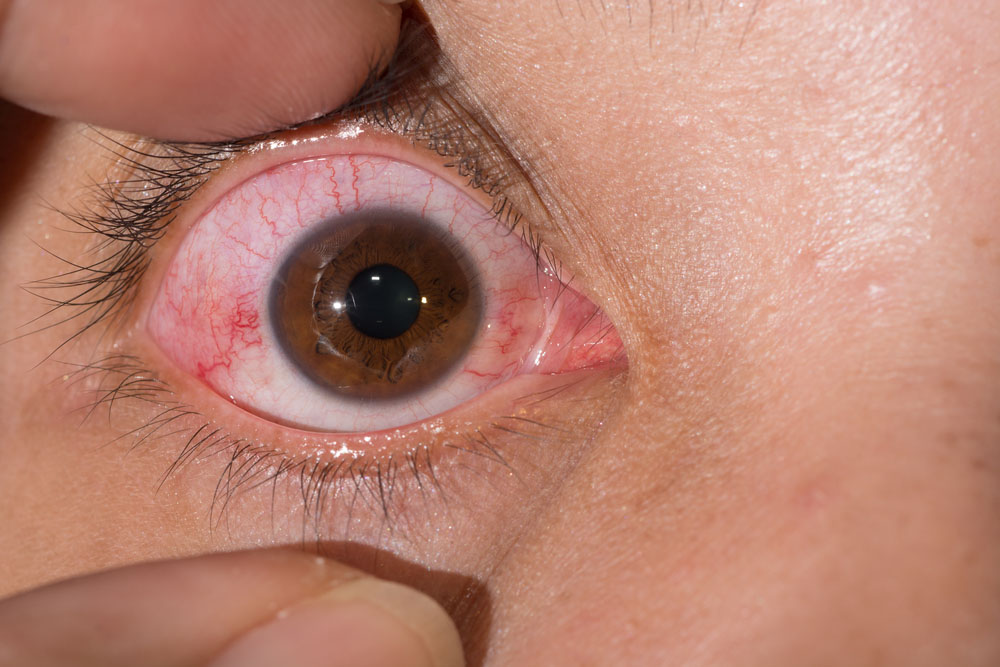
What are the symptoms of scleritis?
Scleritis is an inflammatory condition affecting the sclera, the white outer coating of the eye. The symptoms can vary in severity but typically include:
- Eye Pain: Often described as deep, aching, or throbbing pain that may worsen with eye movement.
- Redness: Redness of the eye, especially around the sclera. The redness can be localized or more widespread.
- Swelling: Swelling of the sclera or surrounding tissues may occur.
- Tearing: Increased tear production or watery eyes.
- Sensitivity to Light (Photophobia): Discomfort or pain when exposed to bright light.
- Vision Changes: Blurred vision or decreased vision in some cases, depending on the extent of inflammation.
- Discharge: Less commonly, there may be a discharge from the eye.
- Eye Warmth: The eye may feel warm to the touch due to inflammation.
Symptoms of scleritis can range from mild to severe and may significantly impact daily activities. If you experience any of these symptoms, especially persistent eye pain or vision changes, it is important to seek medical attention from an ophthalmologist.
What are the causes of scleritis?
Scleritis can be caused by a variety of factors, and it is often associated with underlying systemic conditions. The main causes include:
- Autoimmune Diseases: Conditions such as rheumatoid arthritis, lupus, and granulomatosis with polyangiitis (Wegener’s granulomatosis) can cause scleritis as part of their systemic inflammation.
- Infections: Bacterial, viral, or fungal infections can lead to scleritis. This may occur directly through an eye infection or as a complication of a systemic infection.
- Inflammatory Diseases: Systemic inflammatory conditions like inflammatory bowel disease (e.g., Crohn’s disease or ulcerative colitis) may be associated with scleritis.
- Trauma: Injury to the eye can sometimes trigger inflammation of the sclera.
- Sarcoidosis: This systemic condition, characterized by the formation of granulomas, can cause scleritis.
- Behçet’s Disease: A rare autoimmune condition that can cause inflammation in various parts of the body, including the eyes.
- Systemic Vasculitis: Conditions that involve inflammation of blood vessels, such as giant cell arteritis or polyarteritis nodosa, can lead to scleritis.
- Underlying Health Conditions: Conditions like gout or syphilis may also be associated with scleritis, although less commonly.
In some cases, the cause of scleritis may not be identified, and it can occur without an obvious underlying systemic condition. When scleritis occurs, identifying and treating the underlying cause is crucial for effective management and to prevent complications.
What is the treatment for scleritis?
The treatment for scleritis aims to reduce inflammation, relieve symptoms, and address any underlying conditions. The approach can vary based on the severity of the condition and whether there is an underlying systemic disease. Treatment options include:
- Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs like ibuprofen or prescription NSAIDs can help manage pain and inflammation.
- Corticosteroids: Oral or topical corticosteroids may be prescribed to reduce inflammation, especially for more severe cases. These are usually used when NSAIDs alone are not sufficient.
- Disease-Modifying Antirheumatic Drugs (DMARDs): For scleritis associated with autoimmune diseases, medications such as methotrexate or azathioprine may be used to control the underlying condition.
- Biologic Agents: In some cases, newer biologic drugs like tumor necrosis factor (TNF) inhibitors may be prescribed for autoimmune-related scleritis.
- Treating Underlying Conditions: Managing any underlying systemic disease (such as rheumatoid arthritis or lupus) is crucial for controlling scleritis. This may involve specific treatments targeted at the underlying condition.
- Topical Therapies: For mild cases, eye drops or ointments may be used to reduce inflammation and relieve discomfort.
- Surgical Intervention: Rarely, if there are complications or if the inflammation does not respond to medical treatment, surgical options might be considered.
- Lifestyle and Supportive Measures: Applying cold compresses to the eyes, using artificial tears to alleviate dryness, and avoiding known triggers (like smoking or allergens) can also help manage symptoms.
Regular follow-up with an ophthalmologist or a specialist in autoimmune or inflammatory conditions is essential for monitoring the response to treatment and adjusting the management plan as needed.
Leave a Reply
You must be logged in to post a comment.