What are the symptoms of pudendal neuralgia?
Pudendal neuralgia is characterized by various symptoms associated with nerve dysfunction in the pudendal nerve. These symptoms can include:
- Pelvic Pain: This is often described as a burning, aching, or sharp pain in the pelvic area, particularly around the genitals, perineum, and anus. The pain can be constant or intermittent and may worsen with sitting or other activities.
- Numbness: Some individuals may experience numbness or reduced sensation in the pelvic region.
- Tingling: There may be a tingling or “pins and needles” sensation in the affected area.
- Discomfort During Sitting: Pain or discomfort often increases with prolonged sitting, which is a common symptom due to pressure on the pudendal nerve.
- Pain During Sexual Activity: Individuals may experience pain or discomfort during or after sexual intercourse.
- Pain During Bowel Movements: Pain or discomfort may also be present during or after bowel movements.
- Urinary Issues: Some people may experience urinary problems such as urgency, frequency, or discomfort.
Symptoms can vary in severity and presentation, and they may overlap with other conditions affecting the pelvic region.
What are the causes of pudendal neuralgia?
Pudendal neuralgia can result from various causes that affect the pudendal nerve. These include:
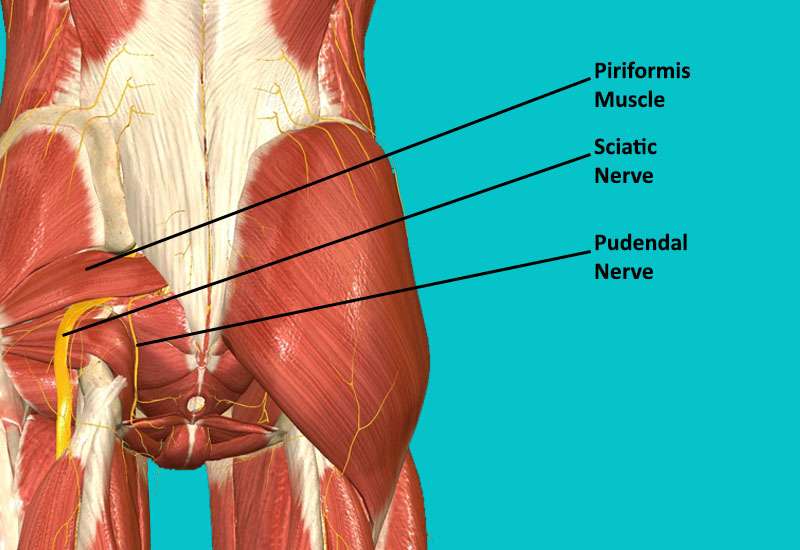
- Nerve Compression: Compression of the pudendal nerve can occur due to pelvic trauma, prolonged sitting, or conditions that create pressure on the nerve, such as pelvic tumors or cysts.
- Childbirth: Trauma during childbirth, such as an extended labor or the use of forceps, can injure or stretch the pudendal nerve.
- Pelvic Surgery: Surgical procedures involving the pelvic region, such as hysterectomy or surgery for prostate cancer, can lead to pudendal nerve damage or irritation.
- Pelvic Trauma: Injuries to the pelvic area, including pelvic fractures or blunt trauma, can affect the pudendal nerve.
- Chronic Prolonged Sitting: Sitting for long periods on hard surfaces can put pressure on the pudendal nerve, leading to nerve irritation or damage.
- Chronic Constipation: Straining during bowel movements due to chronic constipation can put pressure on the pudendal nerve.
- Infections: Infections in the pelvic region, including sexually transmitted infections, can cause inflammation and affect the pudendal nerve.
- Endometriosis: This condition can cause inflammation and scarring in the pelvic area, potentially leading to pudendal nerve irritation.
- Pelvic Floor Dysfunction: Conditions that affect the pelvic floor muscles, such as pelvic floor dysfunction or myofascial pain syndrome, can also contribute to pudendal neuralgia.
- Tumors or Masses: Tumors or other masses in the pelvic region can compress the pudendal nerve, causing symptoms of neuralgia.
In some cases, the exact cause of pudendal neuralgia may not be clear, and it can result from a combination of factors.
What is the treatment for pudendal neuralgia?
The treatment for pudendal neuralgia typically involves a combination of approaches aimed at managing pain and addressing underlying causes. Here’s an overview of common treatments:
Medications:
- Pain relief medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen may be used.
- Neuropathic pain medications, like gabapentin or pregabalin, can help manage nerve pain.
- Antidepressants, particularly tricyclic antidepressants, may be prescribed for pain relief and to improve mood.
Physical Therapy:
- Pelvic floor physical therapy can help alleviate pain by addressing muscle dysfunction and improving pelvic floor strength and flexibility.
- Techniques such as manual therapy, stretching, and strengthening exercises may be included.
Lifestyle Modifications:
- Avoiding prolonged sitting or using cushioned seating to reduce pressure on the pudendal nerve.
- Managing constipation and avoiding straining during bowel movements.
Nerve Blocks and Injections:
- Pudendal nerve blocks can provide temporary pain relief and help diagnose the condition.
- Corticosteroid injections may be used to reduce inflammation and pain.
Surgical Options:
- If conservative treatments fail, surgical interventions may be considered. Surgery might involve decompression of the pudendal nerve or other procedures to address the underlying cause.
Alternative Therapies:
- Acupuncture or chiropractic adjustment might offer additional relief for some individuals.
Psychological Support:
- Therapy or counseling can help manage the emotional impact of chronic pain and improve overall quality of life.
Treatment plans are often individualized, and working closely with a healthcare provider can help determine the most effective approach based on the specific cause and severity of the pudendal neuralgia.
Leave a Reply
You must be logged in to post a comment.