What are the symptoms of pneumococcal disease?
Pneumococcal disease is caused by the bacterium Streptococcus pneumoniae and can lead to a range of infections, each with distinct symptoms. The symptoms vary depending on the type of infection, which can include pneumonia, meningitis, bacteremia, and sinusitis, among others. Here are the symptoms associated with some common forms of pneumococcal disease:
1. Pneumococcal Pneumonia (infection of the lungs):
- Fever and chills
- Cough (may produce greenish or yellow mucus)
- Shortness of breath
- Chest pain (especially when breathing deeply or coughing)
- Fatigue
- Muscle pain
- Headache
- In severe cases, confusion or delirium
2. Pneumococcal Meningitis (infection of the membranes covering the brain and spinal cord):
- High fever
- Severe headache
- Stiff neck
- Sensitivity to light (photophobia)
- Nausea and vomiting
- Confusion or altered mental status
- Seizures
3. Pneumococcal Bacteremia (bacterial infection in the blood):
- Fever and chills
- Low blood pressure
- Rapid heart rate
- Confusion or disorientation
- Septic shock (in severe cases)
4. Pneumococcal Otitis Media (middle ear infection):
- Ear pain
- Fever
- Reduced hearing
- Irritability (especially in children)
- Fluid drainage from the ear
5. Pneumococcal Sinusitis (infection of the sinuses):
- Nasal congestion
- Facial pain or pressure
- Headache
- Fever
- Thick nasal discharge
The severity and specific symptoms can vary depending on the individual’s age, underlying health conditions, and the type of pneumococcal infection. Pneumococcal disease can be serious and requires prompt medical attention. Vaccination is an effective way to prevent many types of pneumococcal infections.
What are the causes of pneumococcal disease?
Pneumococcal disease is caused by the bacterium Streptococcus pneumoniae. This bacterium can lead to various types of infections, and the causes of pneumococcal disease are generally related to how this bacterium spreads and infects individuals. Here are the primary factors:
1. Direct Contact:
- Respiratory Droplets: The bacteria are primarily spread through respiratory droplets from coughing or sneezing. Close contact with an infected person increases the risk of transmission.
2. Colonization:
- Nasal and Throat Carriage: Streptococcus pneumoniae can live harmlessly in the nasopharynx (the upper part of the throat behind the nose) of healthy individuals. In some cases, the bacteria can become pathogenic, especially if the immune system is compromised.
3. Weakened Immune System:
- Immunocompromised Individuals: People with weakened immune systems, such as those with HIV/AIDS, cancer, or chronic illnesses, are more susceptible to pneumococcal infections.
- Older Adults: The immune response can diminish with age, making older adults more vulnerable to pneumococcal disease.
4. Chronic Health Conditions:
- Chronic Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) or asthma can increase the risk of pneumococcal infections.
- Diabetes: People with diabetes may have a higher risk of pneumococcal disease due to compromised immune function.
5. Environmental and Lifestyle Factors:
- Smoking: Smoking damages the respiratory tract and impairs immune function, increasing the risk of pneumococcal infections.
- Crowded Living Conditions: Environments where people are in close proximity, such as daycares or military barracks, can facilitate the spread of Streptococcus pneumoniae.
6. Seasonal Factors:
- Seasonal Variation: Pneumococcal infections may be more common in certain seasons, particularly during winter months when respiratory infections are more prevalent.
7. Age:
- Young Children: Infants and young children are at higher risk due to their developing immune systems and high exposure to other children.
- Older Adults: The elderly are more susceptible due to age-related decline in immune function.
Pneumococcal disease is preventable through vaccination, which is particularly recommended for young children, older adults, and individuals with specific health conditions.
How is the diagnosis of pneumococcal disease made?
The diagnosis of pneumococcal disease is based on a combination of clinical evaluation, medical history, and laboratory tests. The specific diagnostic approach may vary depending on the type of pneumococcal infection. Here’s a general overview of the diagnostic process:
1. Clinical Evaluation:
- Medical History: The healthcare provider will ask about symptoms, their onset, and any recent exposures or health conditions that might increase the risk of pneumococcal disease.
- Physical Examination: A thorough examination is conducted to assess symptoms, such as fever, cough, chest pain, or neurological signs, depending on the type of infection.
2. Laboratory Tests:
- Blood Tests:
- Complete Blood Count (CBC): Can show elevated white blood cell count, which indicates infection or inflammation.
- Blood Cultures: To identify Streptococcus pneumoniae in the bloodstream. This is particularly important in cases of pneumococcal bacteremia or sepsis.
- Sputum Culture: In cases of pneumonia, a sample of sputum (mucus coughed up from the lungs) is collected and cultured to identify the bacteria causing the infection.
- Urinary Antigen Test: This test detects pneumococcal antigens in the urine. It can be useful for diagnosing pneumococcal pneumonia, particularly in cases where blood or sputum cultures are not feasible.
- Pleural Fluid Analysis: If there is fluid in the pleural space (pleural effusion) due to pneumonia, a sample of this fluid can be analyzed for the presence of Streptococcus pneumoniae.
3. Imaging Studies:
- Chest X-ray: Used to visualize the lungs and diagnose pneumonia. It can show patterns consistent with pneumococcal pneumonia, such as consolidation or infiltrates.
- CT Scan: In some cases, a more detailed imaging study may be required to assess the extent of infection or complications.
4. Lumbar Puncture:
- Cerebrospinal Fluid (CSF) Analysis: In cases of suspected pneumococcal meningitis, a lumbar puncture (spinal tap) is performed to collect and analyze cerebrospinal fluid for the presence of Streptococcus pneumoniae. The CSF can be tested for bacteria, white blood cells, and protein levels.
5. Rapid Diagnostic Tests:
- PCR (Polymerase Chain Reaction): A molecular test that can detect the DNA of Streptococcus pneumoniae in clinical samples, such as blood, sputum, or CSF. This is useful for confirming the presence of the bacteria.
The choice of diagnostic tests and procedures will depend on the clinical presentation, suspected type of pneumococcal disease, and available resources. Accurate diagnosis is essential for effective treatment and management of pneumococcal infections.
What is the treatment for pneumococcal disease?
The treatment for pneumococcal disease varies depending on the type and severity of the infection. Here’s an overview of the typical treatments for different forms of pneumococcal disease:
1. Pneumococcal Pneumonia:
- Antibiotics: The primary treatment is antibiotic therapy. Common antibiotics used include:
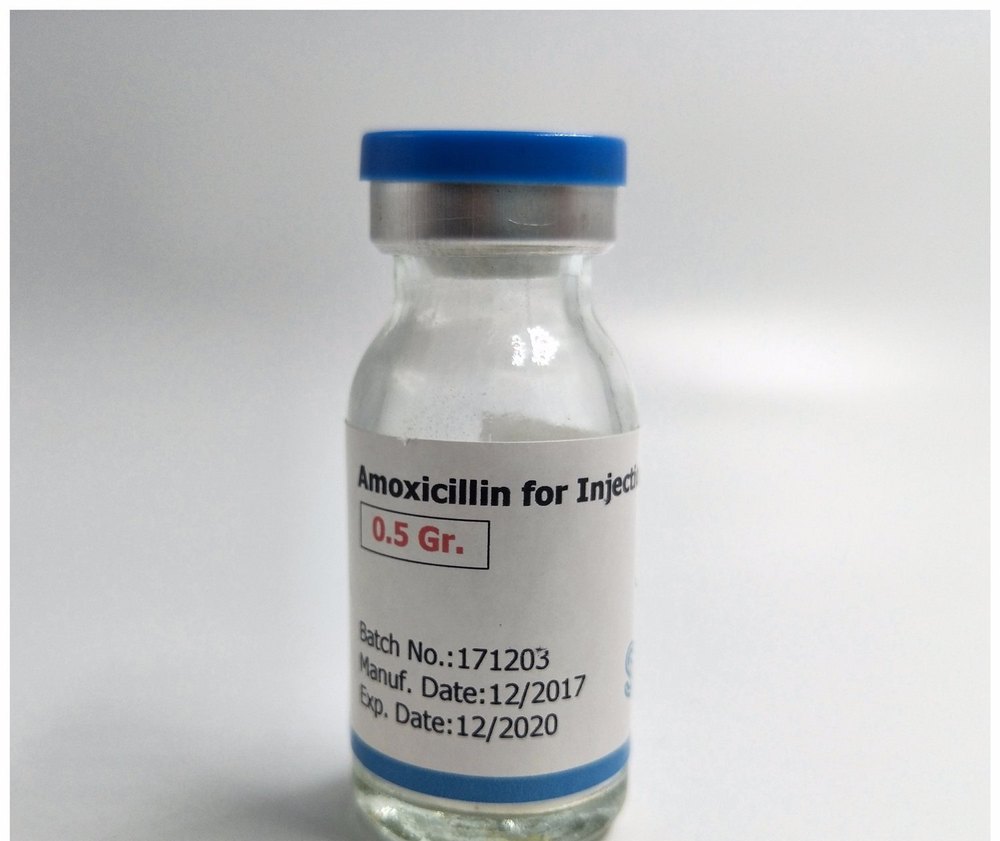
- Penicillin or amoxicillin (often first-line treatments for sensitive strains).
- Macrolides (e.g., azithromycin) or doxycycline (used if the patient is allergic to penicillin or if the strain is resistant).
- Respiratory fluoroquinolones (e.g., levofloxacin) may be used in cases of severe infection or if the patient has other health conditions.
- Supportive Care: This includes rest, hydration, and over-the-counter pain relievers to manage fever and discomfort.
2. Pneumococcal Meningitis:
- Intravenous Antibiotics: Treatment usually involves intravenous antibiotics to penetrate the blood-brain barrier. Common choices include:
- Ceftriaxone or cefotaxime (often combined with vancomycin or rifampin for broader coverage).
- Corticosteroids: In some cases, corticosteroids (e.g., dexamethasone) may be administered to reduce inflammation and improve outcomes.
- Supportive Care: Includes managing symptoms like fever and headache, and monitoring for complications.
3. Pneumococcal Bacteremia:
- Intravenous Antibiotics: Similar to treatment for pneumococcal pneumonia, often with a broad-spectrum antibiotic regimen initially until specific sensitivities are known.
- Supportive Care: Includes fluids, medications to stabilize blood pressure if needed, and treatment of any complications like septic shock.
4. Pneumococcal Otitis Media:
- Antibiotics: Oral antibiotics such as amoxicillin or amoxicillin-clavulanate are commonly used. Treatment may be adjusted based on the child’s response and any local antibiotic resistance patterns.
- Pain Management: Over-the-counter pain relievers and warm compresses can help alleviate discomfort.
5. Pneumococcal Sinusitis:
- Antibiotics: Oral antibiotics like amoxicillin or amoxicillin-clavulanate are typically prescribed. The choice of antibiotic may be adjusted based on the severity of the infection and local resistance patterns.
- Supportive Care: Includes nasal decongestants, saline nasal irrigation, and pain relief.
General Considerations:
- Hospitalization: Severe cases of pneumococcal disease, especially those involving complicated pneumonia, meningitis, or bacteremia, may require hospitalization for intravenous antibiotics and supportive care.
- Vaccination: Preventive vaccination is crucial for reducing the incidence of pneumococcal disease. Vaccines include:
- PCV13 (Pneumococcal Conjugate Vaccine): Recommended for children under 2 years old, adults over 65, and individuals with certain medical conditions.
- PPSV23 (Pneumococcal Polysaccharide Vaccine): Recommended for adults over 65 and those with chronic health conditions or weakened immune systems.
Early diagnosis and appropriate treatment are essential for effective management and reducing the risk of complications. If you suspect pneumococcal disease, it’s important to seek medical attention promptly.
Leave a Reply
You must be logged in to post a comment.