What are the symptoms of Perthes disease?
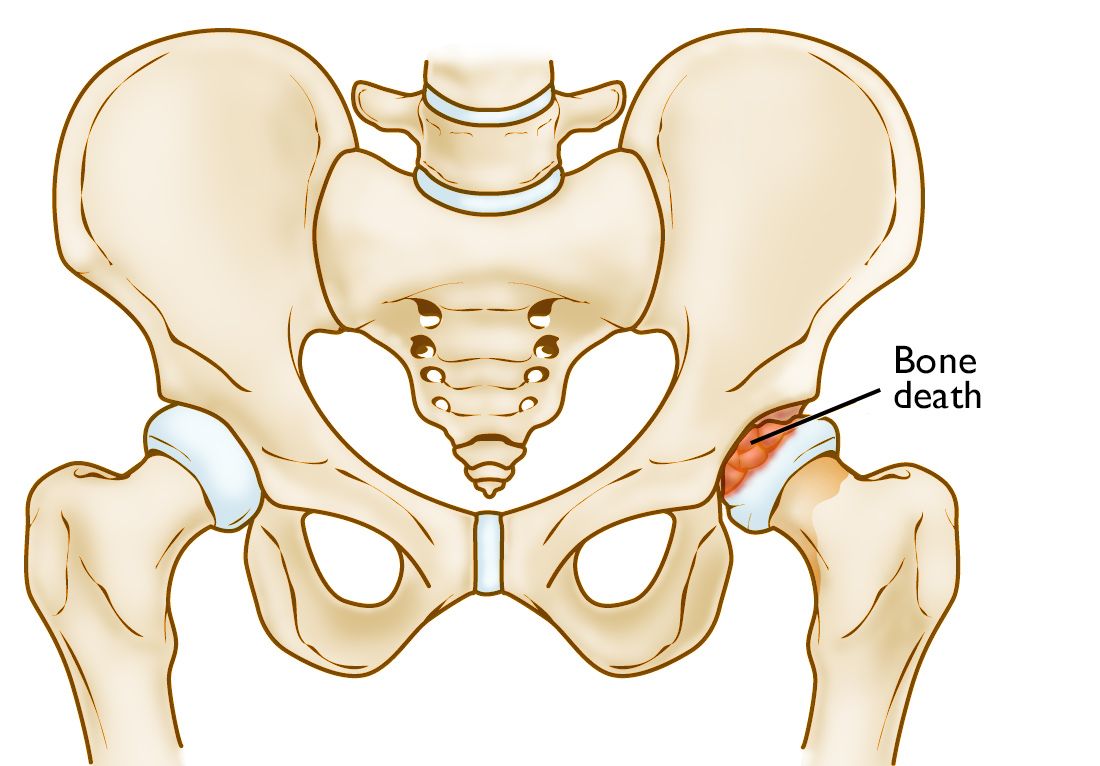
Perthes disease, also known as Legg-Calvé-Perthes disease, is a childhood condition where the blood supply to the femoral head (the ball part of the hip joint) is temporarily disrupted. This leads to the death of the bone tissue (avascular necrosis) and can affect the hip joint’s function. The symptoms of Perthes disease typically include:
Symptoms:
- Pain in the hip joint is the most common symptom. The pain can also be referred to the groin, thigh, or knee.
- Limping:
- Children with Perthes disease often develop a noticeable limp due to discomfort and stiffness in the hip joint.
- Limited Range of Motion:
- Reduced ability to move the hip joint, especially when attempting to rotate or abduct (move the leg away from the body).
- Stiffness:
- The hip joint may feel stiff and resistant to movement, especially after periods of inactivity.
- Muscle Weakness:
- Muscle weakness around the hip can occur due to reduced use of the affected leg.
- Discomfort with Physical Activity:
- Increased pain or discomfort during or after physical activities, such as walking, running, or playing sports.
- Joint Swelling:
- Although less common, there may be some swelling around the hip joint.
Other Considerations:
- Age of Onset:
- Perthes disease typically affects children between the ages of 4 and 8, though it can occur in children as young as 2 or as old as 12.
- Duration:
- Symptoms can vary in duration and severity. The disease often progresses through several stages over a few years.
- Progressive Symptoms:
- The severity of symptoms may change over time as the disease progresses through different phases of bone necrosis and healing.
When to Seek Medical Attention:
- Persistent Pain or Limping:
- If a child experiences ongoing hip pain, limping, or difficulty moving the hip joint, it’s important to consult a healthcare provider.
- Unexplained Symptoms:
- Any unexplained pain or joint stiffness in a child should be evaluated by a physician to rule out Perthes disease or other conditions.
Early diagnosis and treatment are crucial in managing Perthes disease effectively and minimizing potential complications. If you suspect Perthes disease or if your child is exhibiting symptoms, a pediatric orthopedic specialist can provide a thorough evaluation and appropriate management.
What are the causes of Perthes disease?
The exact cause of Perthes disease is not fully understood, but several factors are thought to contribute to its development. Here’s an overview of potential causes and contributing factors:
Potential Causes:
- Disruption of Blood Supply:
- The core issue in Perthes disease is a temporary interruption in the blood supply to the femoral head (the ball of the hip joint). This leads to avascular necrosis (death of bone tissue) and subsequent joint damage.
- Genetic Factors:
- There may be a genetic predisposition to Perthes disease. A family history of the condition or other bone-related disorders may increase the risk, although specific genes or hereditary patterns have not been clearly identified.
- Trauma or Injury:
- Some cases of Perthes disease may follow an injury to the hip or thigh, although this is not always the case. The injury might not directly cause the disease but could be associated with its onset.
- Coagulation Disorders:
- Conditions that affect blood clotting, such as certain blood disorders, might contribute to disruptions in blood flow to the femoral head.
- Inflammation:
- Chronic inflammation or autoimmune conditions might play a role in disrupting blood supply, though this connection is not well-established.
- Biomechanical Factors:
- Abnormalities in hip joint mechanics or alignment could potentially contribute to the development of Perthes disease, although this is less clearly defined.
- Environmental Factors:
- Some researchers suggest that environmental factors, such as exposure to certain toxins or infections, might influence the risk of developing Perthes disease, though more research is needed to confirm these associations.
Key Points:
- Complex Interaction: The development of Perthes disease is likely due to a combination of these factors rather than a single cause.
- Not Directly Preventable: Since the exact causes are not fully understood, there are no known preventative measures for Perthes disease.
- Research and Understanding: Ongoing research aims to better understand the underlying mechanisms and risk factors to improve prevention and treatment strategies.
If you have concerns about Perthes disease or its potential causes, discussing them with a pediatric orthopedic specialist can provide more tailored information and guidance.
How is the diagnosis of Perthes disease made?
The diagnosis of Perthes disease involves a combination of clinical evaluation, imaging studies, and sometimes additional tests to confirm the condition and assess its severity. Here’s a detailed look at the diagnostic process:
1. Clinical Evaluation:
- Medical History:
- The doctor will review the child’s medical history, including any previous injuries, family history of hip or bone conditions, and symptoms experienced (e.g., hip pain, limping, limited range of motion).
- Physical Examination:
- The examination typically focuses on the hip joint to assess pain, range of motion, muscle strength, and any signs of swelling or tenderness. The doctor will observe the child’s gait and may check for any limping or unusual movement patterns.
2. Imaging Studies:
- X-rays:
- Standard X-rays are usually the first imaging test performed. They help identify changes in the shape and structure of the femoral head and hip joint. Early X-rays may appear normal, but as the disease progresses, they can reveal changes such as joint space narrowing, femoral head flattening, or fragmentation.
- MRI (Magnetic Resonance Imaging):
- MRI scans provide detailed images of the bone and soft tissues. They can detect early signs of bone necrosis before these changes become visible on X-rays. MRI is useful for assessing the extent of bone damage and monitoring the progression of the disease.
- CT Scan (Computed Tomography):
- CT scans may be used in some cases to provide more detailed images of the bone structure and assess the degree of femoral head deformation.
- Bone Scintigraphy (Bone Scan):
- This imaging technique involves injecting a small amount of radioactive material to highlight areas of abnormal bone activity. It can help evaluate the blood supply to the femoral head and identify areas of necrosis.
3. Additional Tests:
- Ultrasound:
- Ultrasound may be used to assess joint effusion (fluid accumulation) or to guide certain interventions, although it is not typically used for diagnosing Perthes disease itself.
- Blood Tests:
- While not used to diagnose Perthes disease directly, blood tests might be ordered to rule out other conditions or to check for underlying health issues.
4. Differential Diagnosis:
- Rule Out Other Conditions:
- The doctor will consider and rule out other possible conditions that could present with similar symptoms, such as septic arthritis, osteomyelitis, or other forms of hip joint pathology.
5. Follow-Up:
- Monitoring Progress:
- Regular follow-up visits with imaging studies may be needed to monitor the progression of the disease and assess the effectiveness of treatment.
The diagnosis of Perthes disease typically involves a combination of these methods to ensure an accurate assessment and to develop an appropriate treatment plan. If you suspect Perthes disease in a child, consulting with a pediatric orthopedic specialist is essential for a thorough evaluation and diagnosis.
What is the treatment for Perthes disease?
The treatment for Perthes disease aims to alleviate symptoms, maintain hip joint mobility, and promote the best possible recovery of the femoral head. The approach varies depending on the severity of the disease, the child’s age, and the progression of the condition. Treatment generally includes both non-surgical and surgical options:
Non-Surgical Treatments:
- Observation:
- For mild cases, especially in children who are younger and have less advanced disease, a period of observation may be recommended. Regular follow-ups with imaging studies are used to monitor the condition.
- Activity Modification:
- Limiting weight-bearing activities and high-impact sports to reduce stress on the hip joint. Encouraging low-impact activities, such as swimming, may be advised.
- Physical Therapy:
- A physical therapist may develop a program of exercises to improve hip joint range of motion, strengthen surrounding muscles, and maintain overall mobility.
- Pain Management:
- Over-the-counter pain relievers or anti-inflammatory medications may be prescribed to manage pain and reduce inflammation.
- Orthotic Devices:
- In some cases, the use of hip braces or splints may help maintain proper hip joint alignment and reduce pain.
Surgical Treatments:
- Hip Abduction Bracing:
- For some cases, especially in older children or those with more severe disease, a brace may be used to hold the hip in a position that promotes optimal femoral head development.
- Surgical Interventions:
- Varus Osteotomy: A procedure that involves cutting and realigning the femur to improve the alignment of the hip joint and support the healing process.
- Hip Joint Decompression: A surgical approach to relieve pressure on the femoral head and improve blood flow.
- Femoral Head Resurfacing: In rare cases, this procedure may be used to reshape or replace the femoral head.
Rehabilitation:
- Post-Surgical Rehabilitation:
- After surgery, physical therapy is crucial to restore hip joint function, strength, and flexibility. A tailored rehabilitation program helps ensure the best possible recovery.
Long-Term Management:
- Ongoing Monitoring:
- Regular follow-ups with orthopedic specialists are necessary to monitor the healing process, manage symptoms, and make any adjustments to the treatment plan as needed.
- Supportive Measures:
- Encouraging a balanced diet, maintaining a healthy weight, and engaging in appropriate physical activities are important for overall health and joint function.
Prognosis:
- Recovery:
- The outcome varies depending on the severity of the disease and the effectiveness of the treatment. Many children experience significant improvement and can return to normal activities, though some may have residual issues with hip function.
- Complications:
- Potential complications can include persistent hip stiffness, deformity, or early-onset arthritis. Early and appropriate treatment helps reduce the risk of long-term complications.
If you suspect Perthes disease or have concerns about a child’s hip health, consulting a pediatric orthopedic specialist is essential for an accurate diagnosis and effective treatment plan.
Leave a Reply
You must be logged in to post a comment.