What are the symptoms of peroneal tendonitis?
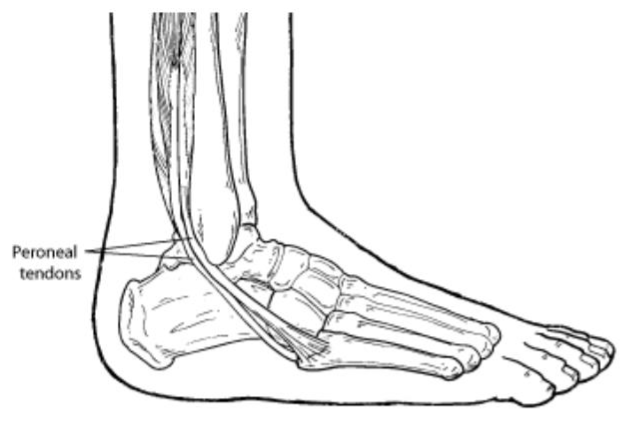
Peroneal tendonitis is an inflammation of the peroneal tendons, which are located on the outer side of the lower leg and help stabilize the ankle. The symptoms of peroneal tendonitis can vary but generally include:
1. Pain:
- Location: Pain is typically felt on the outer side of the ankle or lower leg, where the peroneal tendons are located.
- Intensity: The pain may be sharp or aching and often worsens with activity, particularly activities involving lateral movements or prolonged standing.
2. Swelling:
- Location: Swelling can occur around the outer side of the ankle and may extend up the lower leg.
- Appearance: The area may appear puffy or swollen, and the swelling may be accompanied by warmth.
3. Tenderness:
- Location: Tenderness is usually present along the course of the peroneal tendons, particularly behind the outer ankle bone (lateral malleolus).
- Pressure Sensitivity: The area may be sore to the touch.
4. Stiffness:
- Ankle Movement: Stiffness in the ankle may be present, particularly in the morning or after periods of inactivity.
- Range of Motion: The ability to move the ankle fully may be restricted.
5. Weakness:
- Function: There may be weakness in the ability to stabilize the ankle, leading to difficulties with activities that require lateral movements or balance.
- Movement: Difficulty with foot eversion (turning the foot outward) or pain when attempting to push off with the foot during walking or running.
6. Pain with Activity:
- Exercise or Sports: Pain often intensifies with activities that involve running, jumping, or frequent changes in direction.
- Rest: The pain may improve with rest and worsen with activity.
7. Crepitus:
- Sound: A sensation of crepitus (grating or popping sounds) may be felt or heard during movement, indicating inflammation or irritation of the tendons.
8. Instability:
- Ankle Instability: A feeling of instability or “giving way” in the ankle, particularly when walking on uneven surfaces or engaging in activities that stress the ankle.
Summary:
Symptoms of peroneal tendonitis include pain on the outer side of the ankle or lower leg, swelling, tenderness, stiffness, weakness, pain with activity, crepitus, and possible ankle instability. If you experience these symptoms, it is important to seek medical evaluation for accurate diagnosis and appropriate treatment.
What are the causes of peroneal tendonitis?
Peroneal tendonitis is caused by inflammation of the peroneal tendons, which are responsible for stabilizing and moving the foot. The condition can arise from various factors, often involving a combination of mechanical stress and underlying issues. Here are the common causes:
1. Overuse and Repetitive Strain:
- Excessive Activity: Repeated stress on the peroneal tendons from high-impact activities like running, jumping, or sports involving lateral movements can lead to tendonitis.
- Sudden Increase in Activity: Rapidly increasing the intensity or volume of physical activity without proper conditioning can strain the tendons.
2. Improper Footwear:
- Inadequate Support: Wearing shoes that lack proper arch support or cushioning can place excessive stress on the peroneal tendons.
- Incorrect Fit: Shoes that are too tight or too loose may contribute to improper foot mechanics and increased strain on the tendons.
3. Biomechanical Issues:
- Foot Structure Abnormalities: Structural abnormalities such as high arches (pes cavus) or flat feet (pes planus) can alter the way forces are distributed across the foot, leading to increased stress on the peroneal tendons.
- Overpronation: Excessive inward rolling of the foot (overpronation) can strain the peroneal tendons as they work harder to stabilize the foot.
4. Previous Injuries:
- Prior Ankle Sprains: A history of ankle sprains or injuries can lead to weakness or instability in the peroneal tendons, making them more susceptible to inflammation.
- Tendon Damage: Previous damage or degeneration of the tendons may increase the risk of developing tendonitis.
5. Weakness and Imbalances:
- Muscle Weakness: Weakness in the muscles surrounding the ankle and foot, such as the calf muscles or tibialis muscles, can put additional strain on the peroneal tendons.
- Muscle Imbalances: Imbalances between the muscles on the inner and outer sides of the lower leg can contribute to tendonitis.
6. Abnormal Gait or Mechanics:
- Poor Technique: Incorrect running or walking techniques, such as improper foot strike or gait abnormalities, can increase stress on the peroneal tendons.
- Gait Changes: Alterations in gait due to injury or changes in movement patterns can impact tendon stress.
7. Repetitive Trauma:
- Occupational Stress: Jobs or activities that require repetitive ankle movements or standing for long periods can contribute to the development of peroneal tendonitis.
8. Inflammation or Irritation:
- Tendon Overuse: Chronic irritation or overuse of the peroneal tendons can lead to inflammation and tendonitis.
- Direct Trauma: A direct blow or trauma to the outer ankle or lower leg can cause inflammation in the peroneal tendons.
Summary:
The causes of peroneal tendonitis often involve a combination of overuse, improper footwear, biomechanical issues, previous injuries, weakness, and gait abnormalities. Identifying and addressing these contributing factors is essential for effective treatment and prevention of the condition.
How is the diagnosis of peroneal tendonitis made?
Diagnosing peroneal tendonitis involves a combination of clinical evaluation, imaging studies, and sometimes diagnostic tests. Here’s a step-by-step approach to how the diagnosis is typically made:
1. Clinical Evaluation:
- Medical History:
- Injury History: Discuss any recent injuries, trauma, or activities that might have led to the symptoms.
- Symptom Review: Ask about the onset, location, and nature of the pain, as well as any aggravating or relieving factors.
- Physical Examination:
- Inspection: Look for signs of swelling, bruising, or deformity around the outer ankle and lower leg.
- Palpation: Feel for tenderness along the course of the peroneal tendons, which run behind the outer ankle bone (lateral malleolus).
- Functional Tests: Assess the strength, range of motion, and stability of the ankle. Specific tests may include:
- Resisted Eversion Test: Checking for pain or weakness when the foot is pushed outward against resistance.
- Palpation of Tendons: Feeling along the peroneal tendons for tenderness or swelling.
2. Imaging Studies:
- Ultrasound:
- Purpose: To visualize the peroneal tendons in real-time and assess for inflammation, tears, or degeneration.
- Findings: Can reveal changes in tendon structure, such as thickening or fluid accumulation.
- Magnetic Resonance Imaging (MRI):
- Purpose: To provide detailed images of the tendons and surrounding tissues.
- Findings: MRI can identify tendonitis, tears, and other soft tissue abnormalities. It is particularly useful for assessing the extent of the injury.
- X-rays:
- Purpose: To rule out bony abnormalities or fractures that might be associated with or contributing to the tendon pain.
- Findings: X-rays do not show soft tissues but can help in identifying bony changes or associated injuries.
3. Diagnostic Tests:
- Dynamic Ultrasound:
- Purpose: To assess the tendons during movement and evaluate their function and response to stress.
- Findings: Can help identify issues like tendon subluxation or abnormal movement patterns that may not be visible in static imaging.
4. Differential Diagnosis:
- Evaluation of Other Conditions:
- Purpose: To rule out other potential causes of similar symptoms, such as ankle sprains, ligament injuries, or other tendon issues.
- Approach: Comprehensive assessment of the clinical presentation and imaging results to differentiate between possible conditions.
Summary:
The diagnosis of peroneal tendonitis typically begins with a detailed clinical evaluation, including medical history and physical examination. Imaging studies, such as ultrasound and MRI, are essential for visualizing the tendons and assessing the extent of inflammation or injury. X-rays and dynamic ultrasound may be used to rule out other issues and further evaluate tendon function. Accurate diagnosis helps guide appropriate treatment and management of the condition.
What is the treatment for peroneal tendonitis?
The treatment for peroneal tendonitis aims to reduce pain and inflammation, promote healing, and restore function. Treatment typically involves a combination of conservative management strategies and, in some cases, more advanced interventions. Here’s a comprehensive approach:
1. Rest and Activity Modification:
- Rest:
- Purpose: To reduce strain on the peroneal tendons and allow for healing.
- Method: Avoid activities that exacerbate symptoms, such as running or jumping.
- Activity Modification:
- Purpose: To prevent further irritation of the tendons.
- Method: Substitute high-impact activities with low-impact exercises like swimming or cycling.
2. Ice Therapy:
- Purpose: To reduce swelling and alleviate pain.
- Method: Apply ice packs to the affected area for 15-20 minutes several times a day, particularly after activities that aggravate symptoms.
3. Pain Management:
- Medications:
- Purpose: To control pain and inflammation.
- Method: Use over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen. In some cases, a doctor may prescribe stronger medications.
4. Physical Therapy:
- Purpose: To strengthen the peroneal tendons and surrounding muscles, improve flexibility, and restore function.
- Method:
- Exercises: Focus on strengthening the peroneal muscles, improving ankle stability, and enhancing range of motion.
- Manual Therapy: Techniques like massage and stretching to relieve tension and improve tendon mobility.
- Proprioceptive Training: Exercises to enhance balance and coordination.
5. Orthotic Devices:
- Purpose: To support proper foot alignment and reduce stress on the tendons.
- Method: Use custom-made or off-the-shelf foot orthotics, such as insoles or ankle supports, to provide cushioning and stability.
6. Compression:
- Purpose: To reduce swelling and support the affected area.
- Method: Use compression wraps or sleeves to provide gentle pressure and support.
7. Heat Therapy:
- Purpose: To relax muscles and improve blood flow after the acute inflammation phase has subsided.
- Method: Apply heat packs to the affected area for 15-20 minutes, particularly if stiffness is present.
8. Stretching and Strengthening:
- Purpose: To maintain flexibility and strength in the peroneal tendons and surrounding muscles.
- Method: Incorporate stretching exercises for the calf and Achilles tendon, as well as strengthening exercises for the ankle and lower leg.
9. Surgical Intervention:
- Purpose: For severe cases where conservative measures fail, or if there are significant tears or structural damage.
- Method: Surgical options may include:
- Tendon Repair: Reconstructing or repairing damaged tendons.
- Decompression: Relieving pressure on the tendons if there is associated compression or impingement.
10. Post-Surgical Rehabilitation:
- Purpose: To support recovery and restore function following surgery.
- Method: Follow a structured rehabilitation program, including physical therapy, to regain strength, flexibility, and function.
11. Long-Term Management:
- Ongoing Exercise:
- Purpose: To maintain strength and flexibility and prevent future injuries.
- Method: Continue with a regular exercise routine, including stretching and strengthening exercises.
- Footwear Adjustments:
- Purpose: To provide adequate support and reduce stress on the tendons.
- Method: Wear well-fitting shoes with proper arch support and cushioning.
Summary:
Treatment for peroneal tendonitis involves a combination of rest, ice therapy, pain management, physical therapy, and possibly orthotic devices. In severe cases, surgical intervention may be necessary. Long-term management includes ongoing exercise and proper footwear to prevent recurrence and support overall ankle health.
Leave a Reply
You must be logged in to post a comment.