What are the symptoms of peripheral artery disease?
Peripheral artery disease (PAD) is a condition in which the arteries that supply blood to the limbs, typically the legs, become narrowed or blocked due to atherosclerosis (buildup of fatty deposits and plaque). The symptoms of PAD can vary depending on the severity of the condition. Here are the common symptoms and signs associated with PAD:
1. Claudication:
- Definition: Pain, cramping, or weakness in the legs or buttocks that occurs during physical activity, such as walking or climbing stairs, and is relieved with rest.
- Location: Typically affects the calves, thighs, or buttocks.
2. Rest Pain:
- Description: Pain in the feet or toes that occurs while at rest, especially at night or when lying down. This pain is often relieved by dangling the legs over the side of the bed or walking around.
3. Non-Healing Wounds or Ulcers:
- Description: Sores or wounds on the legs, feet, or toes that do not heal properly or take a long time to heal.
4. Cold Feet or Legs:
- Description: Feet or legs that feel cold compared to the rest of the body, particularly in a warm environment.
5. Changes in Skin Color:
- Description: The skin on the legs or feet may appear pale, bluish, or reddish, depending on the severity of blood flow reduction.
6. Weak or Absent Pulse:
- Description: Weak or absent pulses in the legs or feet, which can be detected during a physical examination by a healthcare provider.
7. Changes in Nail Growth:
- Description: Toenails may become thickened or grow more slowly.
8. Gangrene:
- Description: In severe cases of PAD, lack of blood flow can lead to tissue death (gangrene), which may require amputation of the affected limb.
9. Erectile Dysfunction:
- Description: PAD can also cause erectile dysfunction in men, as the condition affects blood flow to various parts of the body.
Additional Symptoms in Severe Cases:
- Severe Pain at Rest: Especially in the toes or feet, which is not relieved by movement or changing position.
- Critical Limb Ischemia: A condition where the blood flow is severely reduced, leading to persistent pain, non-healing ulcers, and tissue damage.
Summary:
Symptoms of PAD primarily relate to reduced blood flow to the legs and feet, leading to pain, cramping, and other issues during physical activity and at rest. If you experience any of these symptoms, it’s important to seek medical evaluation and treatment. Early diagnosis and management can help alleviate symptoms, improve quality of life, and reduce the risk of complications.
What are the causes of peripheral artery disease?
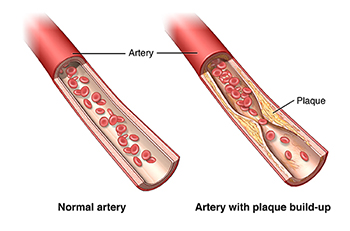
Peripheral artery disease (PAD) is primarily caused by atherosclerosis, a condition where fatty deposits (plaque) build up inside the arteries, leading to reduced blood flow. Several factors contribute to the development of PAD, including:
1. Atherosclerosis:
- Description: The primary cause of PAD. Plaque formed from cholesterol, fats, and other substances accumulates on the arterial walls, narrowing and hardening the arteries, which reduces blood flow to the limbs.
2. Risk Factors:
Lifestyle Factors:
- Smoking:
- Impact: Smoking damages blood vessels, promotes plaque buildup, and reduces blood flow, significantly increasing the risk of PAD.
- Poor Diet:
- Impact: Diets high in saturated fats, trans fats, and cholesterol can lead to plaque formation in the arteries.
- Physical Inactivity:
- Impact: Lack of exercise contributes to obesity and poor cardiovascular health, increasing the risk of PAD.
Medical Conditions:
- Diabetes:
- Impact: High blood sugar levels damage blood vessels and nerves, accelerating the development of PAD.
- Hypertension (High Blood Pressure):
- Impact: Increased pressure can damage arterial walls and promote the development of atherosclerosis.
- High Cholesterol:
- Impact: Elevated levels of LDL (bad cholesterol) and low levels of HDL (good cholesterol) contribute to plaque buildup in the arteries.
- Obesity:
- Impact: Excess body weight puts additional strain on the cardiovascular system and can contribute to the development of PAD.
- Chronic Kidney Disease:
- Impact: Kidney dysfunction is associated with higher levels of atherosclerosis and PAD risk.
Genetic Factors:
- Family History:
- Impact: A family history of cardiovascular diseases or PAD increases the risk of developing the condition.
Other Contributing Factors:
- Age:
- Impact: The risk of PAD increases with age, particularly after age 50.
- Gender:
- Impact: Men are generally at higher risk for PAD, but women with PAD often have more severe disease.
- Inflammation:
- Impact: Chronic inflammation in the body may contribute to the development and progression of atherosclerosis.
- Hormonal Factors:
- Impact: Changes in hormone levels, particularly estrogen, may influence the development of PAD. Women post-menopause may have an increased risk.
Summary:
The primary cause of peripheral artery disease is atherosclerosis, driven by a combination of lifestyle factors, medical conditions, and genetic predispositions. Effective management of PAD involves addressing these risk factors through lifestyle modifications, medication, and medical interventions to prevent progression and manage symptoms. If you have any of the risk factors for PAD, it’s important to discuss them with a healthcare provider for appropriate screening and preventive measures.
How is the diagnosis of peripheral artery disease made?
The diagnosis of peripheral artery disease (PAD) involves a combination of clinical evaluation, medical history, and diagnostic tests. The goal is to confirm the presence of PAD, assess the severity, and rule out other potential conditions. Here’s a step-by-step approach to diagnosing PAD:
1. Clinical Evaluation:
- Patient History:
- Review of symptoms such as leg pain, cramping, or weakness during physical activity (claudication), as well as any history of non-healing wounds or ulcers.
- Assessment of risk factors like smoking, diabetes, hypertension, and high cholesterol.
- Physical Examination:
- Inspection: Check for signs of PAD, including changes in skin color, temperature, or texture, as well as the presence of ulcers or sores.
- Palpation: Feel for pulses in the legs and feet. Weak or absent pulses can indicate reduced blood flow.
- Auscultation: Listen for abnormal sounds, such as bruits (whooshing sounds) over the arteries, which can indicate turbulence due to plaque.
2. Diagnostic Tests:
- Ankle-Brachial Index (ABI):
- Purpose: A key test for diagnosing PAD. It compares the blood pressure in the ankle to the blood pressure in the arm.
- Procedure: Blood pressures are measured in the arm and at the ankle using a Doppler ultrasound device. The ABI is calculated as the ratio of the ankle pressure to the arm pressure.
- Interpretation: An ABI value less than 0.90 is indicative of PAD. Lower values suggest more severe PAD.
- Doppler Ultrasound:
- Purpose: To visualize blood flow in the arteries and identify any blockages or narrowing.
- Procedure: Uses sound waves to create images of blood vessels and assess blood flow and velocity.
- Segmental Pressure Measurements:
- Purpose: To measure blood pressure at different segments of the leg to identify areas of reduced blood flow.
- Procedure: Multiple blood pressure measurements are taken along the legs using a Doppler ultrasound.
- Exercise Testing:
- Purpose: To assess the presence and severity of claudication by measuring the distance a patient can walk before experiencing pain.
- Procedure: The patient walks on a treadmill while symptoms and the time to onset of pain are recorded.
- Imaging Studies:
- Magnetic Resonance Angiography (MRA):
- Purpose: Provides detailed images of blood vessels using magnetic fields and radio waves.
- Computed Tomography Angiography (CTA):
- Purpose: Uses X-rays and computer technology to create detailed images of blood vessels.
- Contrast Angiography:
- Purpose: Involves injecting a contrast dye into the blood vessels and taking X-rays to visualize blockages or narrowing.
3. Blood Tests:
- Lipid Profile:
- Purpose: To evaluate cholesterol levels and assess the risk of atherosclerosis.
- Blood Glucose Levels:
- Purpose: To check for diabetes or prediabetes, which can contribute to PAD.
- Inflammatory Markers:
- Purpose: To assess for systemic inflammation, which may be associated with PAD.
4. Differential Diagnosis:
- Rule Out Other Conditions:
- Conditions such as venous insufficiency, neuropathy, or musculoskeletal issues can mimic PAD symptoms. Diagnostic tests help differentiate PAD from these conditions.
5. Follow-Up and Monitoring:
- Regular Assessments:
- Monitoring the progression of PAD and the effectiveness of treatment through follow-up visits and repeat diagnostic tests if necessary.
Summary:
The diagnosis of peripheral artery disease involves a comprehensive approach that includes a detailed patient history, physical examination, and several diagnostic tests such as the ABI, Doppler ultrasound, and imaging studies. Early and accurate diagnosis is crucial for effective management and to prevent complications associated with PAD. If PAD is suspected, consultation with a healthcare provider is essential for appropriate evaluation and treatment planning.
What is the treatment for peripheral artery disease?
The treatment for peripheral artery disease (PAD) aims to relieve symptoms, improve quality of life, and reduce the risk of cardiovascular events. The approach typically involves a combination of lifestyle changes, medications, and, in some cases, surgical or interventional procedures. Here’s a comprehensive overview of treatment options for PAD:
1. Lifestyle Modifications:
- Smoking Cessation:
- Purpose: Smoking is a major risk factor for PAD and quitting can slow the progression of the disease and improve symptoms.
- Regular Exercise:
- Purpose: Structured exercise programs, such as supervised walking programs, can improve walking distance and reduce symptoms of claudication.
- Recommendation: Aim for at least 30 minutes of moderate-intensity exercise, such as walking, most days of the week.
- Healthy Diet:
- Purpose: A diet low in saturated fats, cholesterol, and sodium can help manage blood pressure and cholesterol levels.
- Recommendation: Focus on a balanced diet with plenty of fruits, vegetables, whole grains, and lean proteins.
- Weight Management:
- Purpose: Maintaining a healthy weight helps reduce the strain on the cardiovascular system and can improve overall health.
2. Medications:
- Antiplatelet Agents:
- Purpose: To prevent blood clots and reduce the risk of heart attack and stroke.
- Examples: Aspirin, clopidogrel.
- Statins:
- Purpose: To lower cholesterol levels and reduce the risk of cardiovascular events.
- Examples: Atorvastatin, simvastatin.
- Medications for Blood Pressure Control:
- Purpose: To manage high blood pressure and reduce cardiovascular risk.
- Examples: ACE inhibitors, ARBs, beta-blockers.
- Medications for Pain Relief:
- Purpose: To alleviate symptoms of claudication.
- Examples: Cilostazol (a vasodilator that can improve walking distance).
- Medications for Diabetes Management:
- Purpose: To control blood sugar levels in diabetic patients.
- Examples: Metformin, insulin.
3. Medical Procedures:
- Angioplasty and Stenting:
- Purpose: To open narrowed or blocked arteries and improve blood flow.
- Procedure: A balloon catheter is used to widen the artery, and a stent may be placed to keep it open.
- Endarterectomy:
- Purpose: To remove plaque from the artery and restore blood flow.
- Procedure: Surgical removal of plaque from the artery.
- Bypass Surgery:
- Purpose: To create an alternate route for blood flow around a blocked or narrowed artery.
- Procedure: A graft is used to bypass the blocked segment of the artery.
4. Monitoring and Follow-Up:
- Regular Check-Ups:
- Purpose: To monitor the progression of PAD and the effectiveness of treatment.
- Tests: Regular assessment through ABI, ultrasound, and other diagnostic tests.
5. Management of Comorbid Conditions:
- Diabetes Management:
- Purpose: To control blood sugar levels and reduce the risk of complications.
- Blood Pressure Management:
- Purpose: To keep blood pressure within a healthy range and reduce cardiovascular risk.
- Cholesterol Management:
- Purpose: To control lipid levels and prevent further plaque buildup.
6. Patient Education:
- Self-Care:
- Purpose: To educate patients about managing symptoms, recognizing complications, and adhering to treatment plans.
- Foot Care:
- Purpose: To prevent complications such as ulcers and infections, especially in patients with diabetes.
Example Treatment Plan:
For a patient with mild PAD:
- Lifestyle Changes: Smoking cessation, regular exercise, healthy diet.
- Medications: Aspirin, statins, cilostazol.
- Follow-Up: Regular ABI measurements and check-ups.
For a patient with severe PAD:
- Lifestyle Changes: As above, with more emphasis on intensive management.
- Medications: As above, with additional medications for pain relief and blood pressure control.
- Medical Procedures: Consideration of angioplasty, stenting, or bypass surgery based on severity and symptoms.
Summary:
The treatment for peripheral artery disease involves a multifaceted approach that includes lifestyle modifications, medications, and, when necessary, medical or surgical interventions. Effective management can significantly improve symptoms, enhance quality of life, and reduce the risk of serious cardiovascular events. Regular follow-up with a healthcare provider is essential for optimizing treatment and monitoring progress.
Leave a Reply
You must be logged in to post a comment.