What are the symptoms of periodontal disease?
Periodontal disease, also known as gum disease, can vary in severity from gingivitis to more advanced periodontitis. Symptoms of periodontal disease include:
Early Stage (Gingivitis):
- Red or Swollen Gums: The gums may appear red, swollen, or inflamed.
- Bleeding Gums: Gums may bleed during brushing, flossing, or eating hard foods.
- Bad Breath: Persistent bad breath or a bad taste in the mouth.
- Tenderness: Gums may feel tender or sensitive to touch.
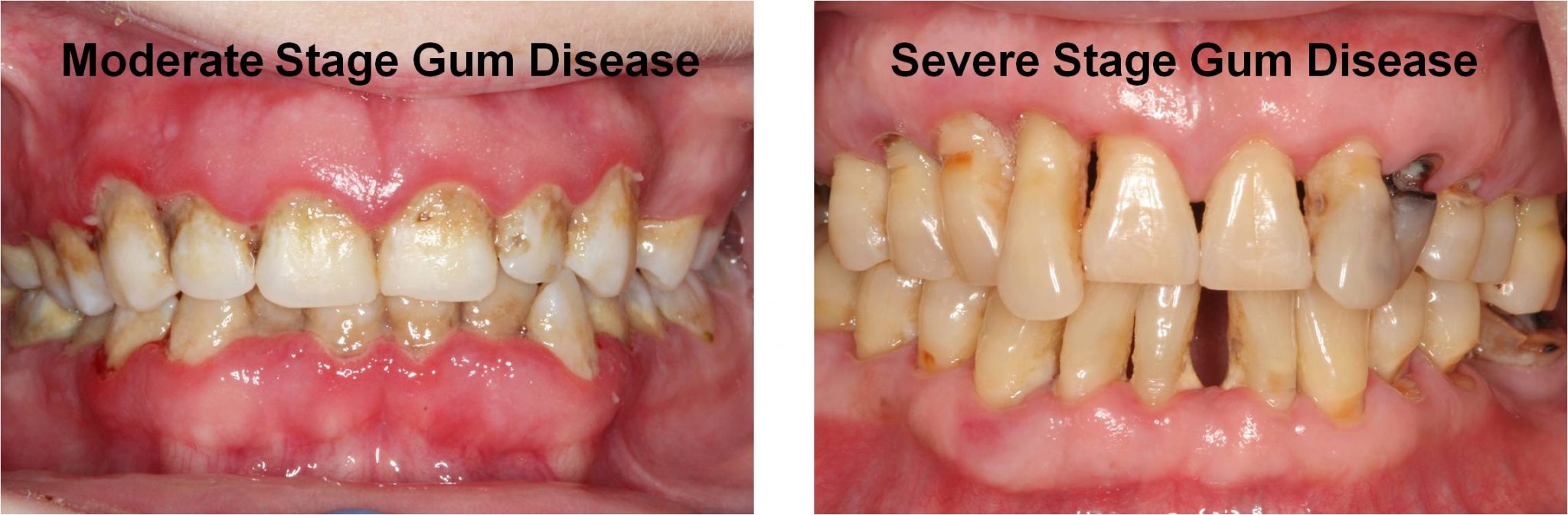
Advanced Stage (Periodontitis):
- Gum Recession: The gums may begin to pull away from the teeth, exposing more of the tooth or its root.
- Deepening Pockets: The spaces between the teeth and gums (gum pockets) may become deeper and fill with bacteria and plaque.
- Loose Teeth: Teeth may become loose or shift in position due to the loss of supporting bone and gum tissue.
- Persistent Bad Breath: Bad breath may worsen as the infection progresses.
- Gum Abscesses: Abscesses or pus-filled pockets may develop around the teeth.
- Pain: Gums may be painful, especially when eating or brushing.
- Changes in Bite: Changes in the way the teeth fit together when biting or chewing.
- Tooth Sensitivity: Increased sensitivity to hot, cold, or sweet foods and drinks.
General Symptoms:
- Unpleasant Taste: A bad taste in the mouth, often due to the presence of infected gum tissue or pus.
- Plaque or Tartar Buildup: Visible buildup of plaque or tartar along the gumline.
Additional Symptoms (in severe cases):
- Swollen Lymph Nodes: In advanced cases, swollen lymph nodes in the neck or jaw may occur as a response to infection.
- Fever: Occasionally, fever may develop if the infection spreads or becomes severe.
If you experience any of these symptoms, it’s important to seek dental care for an accurate diagnosis and appropriate treatment. Early intervention can help prevent the progression of periodontal disease and manage its effects effectively.
What are the causes of periodontal disease?
Periodontal disease, commonly referred to as gum disease, is primarily caused by bacterial infections that affect the structures surrounding the teeth, including the gums, periodontal ligament, and alveolar bone. While bacterial plaque is the main culprit, various other factors contribute to the development and progression of the disease. Below is a detailed overview of the causes of periodontal disease:
1. Bacterial Plaque Buildup
- Cause: Plaque is a sticky film of bacteria that constantly forms on the teeth and gums. If not removed through proper brushing and flossing, it can lead to periodontal disease.
- Mechanism: Plaque bacteria release toxins that irritate the gum tissue, causing inflammation (gingivitis). As the condition worsens, bacteria move below the gumline, leading to the destruction of gum tissue and bone, eventually resulting in periodontitis if left untreated.
- Consequence: Plaque buildup is the primary initiator of periodontal disease. Without regular dental care and good oral hygiene, plaque can harden into tartar, which cannot be removed by brushing alone.
2. Tartar (Calculus) Formation
- Cause: When plaque is not removed, it hardens and becomes tartar (calculus), which can form above and below the gumline.
- Mechanism: Tartar is a rough surface that allows more plaque to accumulate. It also irritates the gums, exacerbating inflammation. Over time, tartar buildup can cause the gums to pull away from the teeth, creating pockets where bacteria can thrive and cause deeper infections.
- Consequence: Tartar buildup makes it more difficult to clean the teeth properly and requires professional dental cleaning to remove it. Its presence accelerates the progression of gum disease.
3. Poor Oral Hygiene
- Cause: Inadequate brushing and flossing allow plaque and tartar to accumulate, leading to gum inflammation and infection.
- Mechanism: Without regular cleaning, bacteria in the plaque continue to thrive and release toxins that damage the gums. Over time, the gums recede, and the infection can spread deeper into the supporting structures of the teeth.
- Consequence: Poor oral hygiene is one of the leading risk factors for developing periodontal disease. It directly contributes to the buildup of plaque and tartar, which causes inflammation and tissue destruction.
4. Smoking and Tobacco Use
- Cause: Smoking and using other forms of tobacco significantly increase the risk of periodontal disease.
- Mechanism: Tobacco reduces blood flow to the gums, impairing the immune response and the body’s ability to fight infections. It also promotes bacterial growth in the mouth and impairs the healing of gum tissues.
- Consequence: Smokers are at a much higher risk of developing periodontal disease. Smoking also reduces the effectiveness of treatments, making it more difficult to control the condition.
5. Genetics
- Cause: Genetics play a role in an individual’s susceptibility to periodontal disease.
- Mechanism: Some people are genetically predisposed to developing gum disease due to their immune response to bacterial infections. Certain genetic variations can make a person more prone to exaggerated inflammatory responses in the gums, even with good oral hygiene.
- Consequence: Individuals with a family history of periodontal disease may be at higher risk and may require more vigilant oral care and regular dental visits.
6. Hormonal Changes
- Cause: Hormonal fluctuations during puberty, pregnancy, menstruation, and menopause can increase the risk of gum disease.
- Mechanism: Changes in hormone levels can make the gums more sensitive to plaque and more prone to inflammation. Pregnancy gingivitis is common, and if left untreated, it can develop into periodontitis.
- Consequence: Women are at higher risk for gum disease during hormonal changes. Extra attention to oral hygiene during these periods can help reduce the risk.
7. Chronic Diseases
- Cause: Chronic conditions, such as diabetes and autoimmune diseases, can increase the risk of developing periodontal disease.
- Mechanism:
- Diabetes: Poorly controlled diabetes weakens the immune system and impairs the body’s ability to fight infections. High blood sugar levels can also promote the growth of harmful bacteria in the mouth, leading to more severe gum inflammation.
- Autoimmune Diseases: Conditions like lupus and rheumatoid arthritis can lead to inflammation throughout the body, including the gums, making them more susceptible to infection.
- Consequence: People with chronic diseases, especially diabetes, are more likely to develop periodontal disease and may experience more severe forms of the condition.
8. Medications
- Cause: Certain medications can affect the health of the gums and contribute to periodontal disease.
- Mechanism:
- Dry Mouth: Medications such as antihistamines, antidepressants, and some blood pressure medications can reduce saliva flow, leading to dry mouth. Saliva is essential for washing away bacteria and food particles, so a lack of saliva increases the risk of plaque buildup.
- Gum Overgrowth: Some medications, such as anti-seizure drugs (e.g., phenytoin) and immunosuppressants (e.g., cyclosporine), can cause the gums to overgrow, making it easier for plaque to accumulate in hard-to-reach areas.
- Consequence: These medications can increase the risk of gum infections, and individuals taking them should be vigilant about maintaining oral hygiene and regular dental care.
9. Weakened Immune System
- Cause: A compromised immune system, such as in individuals with HIV/AIDS, leukemia, or those undergoing cancer treatments, increases the risk of periodontal disease.
- Mechanism: When the immune system is weakened, the body’s ability to fight off bacterial infections in the gums is reduced, making it easier for periodontal disease to develop and progress.
- Consequence: People with weakened immune systems are more susceptible to infections and may need more frequent dental care to prevent or control gum disease.
10. Stress
- Cause: Chronic stress is a risk factor for periodontal disease.
- Mechanism: Stress weakens the immune system, making it harder for the body to fight infections, including gum infections. Stress can also lead to poor oral hygiene habits and increased teeth grinding (bruxism), which can contribute to gum damage.
- Consequence: Individuals under significant stress may be more likely to develop periodontal disease or experience faster progression due to impaired immune function and oral care neglect.
11. Nutritional Deficiencies
- Cause: Poor nutrition, particularly a lack of essential vitamins and minerals, can contribute to gum disease.
- Mechanism: Vitamin C is crucial for maintaining healthy gums and connective tissues. A deficiency in vitamin C can lead to scurvy, which causes gum bleeding and tissue breakdown. Other nutrient deficiencies can weaken the immune system, making the gums more prone to infection.
- Consequence: A diet low in essential nutrients, especially vitamin C, increases the risk of developing periodontal disease and exacerbates its progression.
12. Obesity
- Cause: Being overweight or obese can increase the risk of developing periodontal disease.
- Mechanism: Obesity is associated with systemic inflammation, which can affect the gums and increase susceptibility to bacterial infections. Fat tissue also releases inflammatory chemicals that may contribute to the development of gum disease.
- Consequence: Individuals with obesity may experience more severe periodontal disease due to the chronic inflammation associated with their condition.
13. Teeth Grinding (Bruxism)
- Cause: Bruxism, or grinding and clenching of the teeth, puts excessive pressure on the gums and teeth, contributing to gum disease.
- Mechanism: The excessive force from grinding can damage the periodontal ligament and supporting bone, making the gums more susceptible to bacterial infection.
- Consequence: Bruxism can exacerbate periodontal disease and increase the risk of tooth loss due to the damage it causes to the gum and bone tissue.
14. Poorly Fitting Dental Appliances
- Cause: Ill-fitting dental bridges, dentures, or other dental appliances can contribute to the development of periodontal disease.
- Mechanism: When dental appliances do not fit properly, they can irritate the gums and create areas where plaque and bacteria accumulate, leading to inflammation and infection.
- Consequence: Properly fitting dental appliances are essential to maintaining good oral health and preventing gum disease.
Conclusion
Periodontal disease is primarily caused by the accumulation of bacterial plaque and tartar around the teeth and gums, but many other factors contribute to its development. These include poor oral hygiene, smoking, genetic predisposition, chronic illnesses, hormonal changes, medications, and stress. Proper oral hygiene, regular dental checkups, and addressing these risk factors can help prevent or manage periodontal disease.
How is the diagnosis of periodontal disease made?
The diagnosis of periodontal disease is made through a comprehensive evaluation by a dentist or periodontist. This process involves a combination of patient history, clinical examination, radiographic imaging, and laboratory testing to determine the presence and extent of periodontal disease. Below is a detailed breakdown of how the diagnosis is made:
1. Medical and Dental History
- Patient History: The first step in diagnosing periodontal disease is taking a detailed medical and dental history. The dentist will ask about:
- Symptoms: Pain, swelling, bleeding gums, loose teeth, bad breath, or any changes in the bite.
- Risk Factors: Smoking, diabetes, stress, medications, family history of gum disease, and hormonal changes.
- Oral Hygiene Practices: The frequency and methods of brushing, flossing, and the use of mouth rinses.
- Past Dental Treatments: Any history of gum disease, dental procedures, or dental appliances like dentures, bridges, or braces.
- Relevance: This history helps the dentist assess risk factors that may predispose the patient to periodontal disease and guides the clinical examination.
2. Clinical Examination
- Visual Inspection of Gums:
- Gum Appearance: The dentist will examine the color, texture, and shape of the gums. Healthy gums should be pink and firm, while diseased gums may appear red, swollen, or receding.
- Signs of Inflammation: Bleeding gums, especially when touched or probed, are a key sign of gingivitis or periodontitis.
- Gum Recession: The dentist will check if the gums are pulling away from the teeth, exposing the tooth roots, which is a common sign of advanced periodontal disease.
- Gingival Pocket Depth Measurement:
- Probing: A periodontal probe is gently inserted between the teeth and gums to measure the depth of the gum pockets (spaces between the gum and the tooth).
- Healthy Gums: Pocket depth should be between 1-3 millimeters.
- Gingivitis: Pockets may be slightly deeper, but without significant bone loss.
- Periodontitis: Deeper pockets (4-12 millimeters) indicate the destruction of the periodontal ligament and bone. Deeper pockets signal more severe disease.
- Bleeding on Probing: Bleeding during probing is an important indicator of gum inflammation and infection.
- Relevance: Measuring pocket depth helps determine the severity of gum disease and whether it is limited to the gums (gingivitis) or involves deeper structures (periodontitis).
- Tooth Mobility:
- Checking for Loose Teeth: The dentist will gently move each tooth to assess mobility. Loose teeth indicate that the periodontal support (bone and ligaments) has been damaged.
- Relevance: Tooth mobility is a sign of advanced periodontal disease, where the bone supporting the teeth has been eroded.
- Bite Evaluation (Occlusion):
- Shifting or Misaligned Teeth: The dentist will check for any changes in the way the teeth come together when biting or chewing.
- Relevance: Changes in bite may indicate that the supporting structures of the teeth have been compromised due to periodontal disease.
3. Radiographic Examination (Dental X-Rays)
- Purpose: Dental X-rays are an essential tool for diagnosing periodontal disease because they allow the dentist to assess the health of the bone surrounding the teeth, which cannot be seen during a visual exam alone.
- Types of X-rays Used:
- Bitewing X-rays: These X-rays show the upper and lower teeth in one area of the mouth and are useful for detecting bone loss in early-stage periodontitis.
- Panoramic X-rays: This type provides a broad view of the entire mouth and jaw. It is useful for identifying advanced bone loss and any abnormalities in the jaw.
- Periapical X-rays: These X-rays capture the entire tooth from the crown to the tip of the root, helping assess the extent of bone destruction.
- Findings on X-rays:
- Bone Loss: One of the key indicators of periodontitis is the loss of alveolar bone, which supports the teeth. X-rays help identify the extent and pattern of bone loss.
- Tartar and Plaque: X-rays can also detect hard deposits of tartar (calculus) below the gumline, which contribute to periodontal disease.
- Relevance: Radiographic images are critical for determining the severity of periodontitis and formulating an appropriate treatment plan.
4. Plaque and Tartar Assessment
- Examination of Plaque and Tartar: During the clinical examination, the dentist will assess the amount and location of plaque and tartar buildup on the teeth, especially below the gumline. Plaque is a sticky film of bacteria, while tartar is hardened plaque that contributes to gum irritation.
- Relevance: Excessive plaque and tartar buildup are key contributors to the onset and progression of periodontal disease. Removing them is essential in treatment.
5. Assessment of Gum Recession
- Exposed Tooth Roots: The dentist will check for signs of gum recession, where the gums pull back, exposing the roots of the teeth. This is a sign of advanced gum disease.
- Relevance: Gum recession is often associated with periodontitis and can lead to tooth sensitivity, decay, and tooth loss if not treated.
6. Bacterial Culture or DNA Testing
- Purpose: In some cases, the dentist may take a sample of plaque from beneath the gumline to analyze the types of bacteria present.
- Types of Tests:
- Bacterial Culture: Identifying the specific bacteria responsible for the infection can help tailor treatment. Some strains of bacteria are more aggressive and destructive than others.
- DNA Testing: This newer method can identify the genetic markers of bacteria associated with periodontal disease. DNA testing can also be used to assess genetic susceptibility to periodontal disease.
- Relevance: Knowing the specific bacteria involved allows for more targeted antibiotic therapy or other treatments if necessary.
7. Salivary Diagnostic Testing
- Purpose: Some dentists use salivary tests to measure enzymes and inflammatory markers that indicate active periodontal disease.
- Relevance: Salivary testing is a non-invasive way to detect early signs of gum disease and monitor treatment effectiveness.
8. Gum Tissue Biopsy (in Rare Cases)
- Purpose: If there is suspicion of other conditions, such as oral cancer or a specific type of inflammatory disease, a small sample of gum tissue may be taken and analyzed.
- Relevance: While not common, this test can rule out other diseases that mimic periodontal disease.
Conclusion
The diagnosis of periodontal disease involves a thorough combination of patient history, clinical examination, probing of the gums to assess pocket depth, dental X-rays to evaluate bone loss, and sometimes bacterial or salivary testing to identify specific pathogens. These steps help the dentist determine the stage of the disease (from mild gingivitis to severe periodontitis) and guide the treatment plan.
What is the treatment for periodontal disease?
The treatment for periodontal disease aims to control the infection, reduce inflammation, and prevent further damage to the gums and supporting structures of the teeth. Treatment approaches vary depending on the severity of the disease and may include:
1. Non-Surgical Treatments:
1.1 Scaling and Root Planing (Deep Cleaning):
- Scaling: Removal of plaque and tartar from the tooth surfaces above and below the gumline.
- Root Planing: Smoothing the root surfaces to remove bacteria and toxins, which helps the gums reattach to the tooth.
1.2 Antimicrobial Treatments:
- Topical Antiseptics: Application of antimicrobial agents or antiseptic solutions directly to the gums to help reduce bacterial load.
- Antibiotics: Oral antibiotics may be prescribed to help control infection, especially if the infection is severe or does not respond to initial treatments.
1.3 Improved Oral Hygiene:
- Instruction on Brushing and Flossing: Dentists provide guidance on proper brushing techniques, flossing, and the use of interdental brushes to improve oral hygiene.
- Professional Cleanings: Regular dental cleanings to remove plaque and tartar and monitor gum health.
2. Surgical Treatments:
2.1 Periodontal Surgery:
- Flap Surgery: A procedure where the gums are lifted back to clean deep pockets and then repositioned to fit snugly around the teeth.
- Bone Grafting: If there is significant bone loss, bone grafts may be used to regenerate lost bone and support the teeth.
- Guided Tissue Regeneration: A technique involving the placement of a barrier membrane to help regenerate lost bone and gum tissue.
2.2 Gingival Grafting:
- Soft Tissue Grafts: In cases of severe gum recession, grafts may be used to cover exposed tooth roots and improve gum coverage.
3. Management of Contributing Factors:
3.1 Treatment of Systemic Conditions:
- Management of Diabetes or Other Conditions: Addressing systemic health conditions that can affect gum health and healing.
3.2 Smoking Cessation:
- Support and Resources: Providing resources and support to help patients quit smoking, as tobacco use can exacerbate periodontal disease.
3.3 Adjustments to Dental Restorations:
- Repair or Replacement: Fixing or replacing poorly fitting dental restorations that may contribute to plaque accumulation and gum problems.
4. Ongoing Care:
4.1 Regular Check-Ups:
- Monitoring: Regular dental visits to monitor the condition of the gums, ensure the effectiveness of treatment, and make necessary adjustments.
4.2 Periodontal Maintenance:
- Professional Cleanings: More frequent cleanings may be recommended to maintain gum health and prevent recurrence of periodontal disease.
Effective treatment of periodontal disease often requires a combination of these approaches, tailored to the individual’s needs and the severity of the disease. Early intervention and ongoing care are essential for managing periodontal disease and maintaining overall oral health. If you suspect you have periodontal disease, consult with a dentist or periodontist for a comprehensive evaluation and treatment plan.
Leave a Reply
You must be logged in to post a comment.