What are the symptoms of pediatric and adolescent scoliosis?
Pediatric and adolescent scoliosis is a condition characterized by an abnormal lateral curvature of the spine. The symptoms can vary depending on the severity of the curvature and the age of the child or adolescent. Here are the common symptoms:
1. Visible Signs
- Asymmetrical Shoulders:
- One shoulder may appear higher than the other.
- Uneven Waist:
- The waist may seem uneven, with one side appearing higher or more pronounced.
- Prominent Shoulder Blade:
- One shoulder blade may protrude more than the other.
- Rib Hump:
- A visible hump may be present on one side of the back when bending forward.
- Leaning:
- The entire body may lean to one side.
2. Postural Changes
- Uneven Hips:
- One hip may appear higher or more prominent than the other.
- Trunk Shift:
- The upper body may shift to one side.
- Head Position:
- The head may not be centered over the pelvis.
3. Pain and Discomfort
- Back Pain:
- While scoliosis is often painless, some children and adolescents may experience back pain, particularly if the curvature is severe.
- Muscle Spasms:
- Muscle spasms or discomfort may occur due to the uneven distribution of weight and muscle strain.
4. Respiratory Symptoms (Severe Cases)
- Breathing Difficulties:
- In severe cases, the curvature of the spine may affect lung function, leading to breathing difficulties.
5. Changes in Gait
- Walking:
- An uneven gait or walking pattern may be observed due to the imbalance caused by the spinal curvature.
6. Clothing Fit Issues
- Clothes:
- Clothes may hang unevenly or not fit properly, which can be an early indicator of scoliosis.
7. Lack of Symmetry
- General Asymmetry:
- Overall asymmetry of the body may be noticeable, especially as the child grows.
8. No Symptoms
- Asymptomatic:
- In many cases, especially in mild scoliosis, there may be no noticeable symptoms, and the condition is often discovered during routine physical examinations or school screenings.
Summary
The symptoms of pediatric and adolescent scoliosis can range from visible signs, such as asymmetry in the shoulders, hips, or rib cage, to more subtle indicators like uneven clothing fit. Pain and discomfort are not common but can occur, especially in more severe cases. Early detection through routine check-ups or school screenings is crucial for timely intervention and management. If scoliosis is suspected, it is essential to consult a healthcare provider for proper diagnosis and treatment.
What are the causes of pediatric and adolescent scoliosis?
The causes of pediatric and adolescent scoliosis can vary, and in many cases, the exact cause is not known. The condition can be classified based on its underlying cause or lack thereof. Here are the main types and causes of scoliosis in children and adolescents:
1. Idiopathic Scoliosis
- Unknown Cause:
- Most Common: Idiopathic scoliosis is the most common type, accounting for about 80-85% of cases. The exact cause is unknown, but it is believed to involve a combination of genetic and environmental factors.
- Subtypes:
- Infantile Idiopathic Scoliosis: Occurs in children under 3 years old.
- Juvenile Idiopathic Scoliosis: Occurs in children aged 4 to 10 years.
- Adolescent Idiopathic Scoliosis: Occurs in adolescents aged 11 to 18 years.
2. Congenital Scoliosis
- Structural Abnormalities:
- Birth Defects: Congenital scoliosis results from malformations of the spine that occur during fetal development. These abnormalities can include fused vertebrae or partially formed vertebrae, leading to an uneven spinal curvature.
3. Neuromuscular Scoliosis
- Neurological and Muscular Conditions:
- Associated Disorders: Neuromuscular scoliosis is associated with neurological or muscular conditions that affect the muscles’ ability to support the spine. Conditions include:
- Cerebral Palsy: A group of disorders affecting movement and muscle tone.
- Muscular Dystrophy: A group of genetic diseases causing progressive muscle weakness.
- Spina Bifida: A birth defect where the spine and spinal cord do not form properly.
- Spinal Cord Injuries: Damage to the spinal cord that can affect muscle control and sensation.
4. Syndromic Scoliosis
- Associated Syndromes:
- Genetic Syndromes: Syndromic scoliosis is associated with specific syndromes or genetic conditions, such as:
- Marfan Syndrome: A connective tissue disorder.
- Ehlers-Danlos Syndrome: A group of disorders affecting connective tissues.
- Neurofibromatosis: A genetic disorder causing tumors to form on nerve tissue.
5. Degenerative Scoliosis
- Age-Related Changes:
- Less Common in Children: Although more common in adults, degenerative scoliosis can occasionally affect children with early-onset degenerative diseases. It results from the degeneration of the spinal discs and joints.
6. Functional Scoliosis
- Postural and Environmental Factors:
- Leg Length Discrepancy: This type of scoliosis occurs due to a discrepancy in leg length, causing the spine to curve to compensate.
- Muscle Spasms or Inflammation: Temporary scoliosis can occur due to muscle spasms or inflammation, which cause an imbalance in muscle strength around the spine.
7. Risk Factors and Genetics
- Family History:
- Genetic Predisposition: There is evidence to suggest a genetic component, as scoliosis can run in families.
- Growth Spurts:
- Rapid Growth: Scoliosis often develops during periods of rapid growth, such as during puberty.
Summary
The causes of pediatric and adolescent scoliosis can be diverse, ranging from unknown (idiopathic) to specific conditions like congenital malformations, neuromuscular diseases, and genetic syndromes. Idiopathic scoliosis, the most common form, has no identifiable cause, while congenital and neuromuscular types are associated with structural and systemic conditions. Genetic factors and rapid growth during adolescence are also contributing factors. A comprehensive evaluation by a healthcare provider is necessary to determine the specific cause and appropriate treatment.
How is the diagnosis of pediatric and adolescent scoliosis made?
The diagnosis of pediatric and adolescent scoliosis is typically made through a combination of medical history, physical examination, and imaging studies. The process involves assessing the curvature of the spine, determining its severity, and identifying any underlying causes. Here’s an overview of the diagnostic steps:
1. Medical History
- Family History:
- The healthcare provider may ask about a family history of scoliosis or other spinal conditions, as there can be a genetic predisposition.
- Patient Symptoms:
- Questions about symptoms, such as back pain, asymmetry in the shoulders or hips, or any limitations in physical activity, are discussed.
2. Physical Examination
- Visual Inspection:
- The doctor examines the patient’s back for signs of asymmetry, such as uneven shoulders, a protruding shoulder blade, uneven hips, or a rib hump.
- Forward Bend Test (Adam’s Test):
- The patient is asked to bend forward at the waist with arms hanging down. This position accentuates any rib hump or asymmetry in the back, which is a common sign of scoliosis.
- Measurement of Leg Length:
- The provider checks for leg length discrepancies, which can cause a functional curvature of the spine.
- Palpation and Range of Motion:
- The spine is palpated to check for abnormalities, and the range of motion is assessed to determine if there are any restrictions or discomfort.
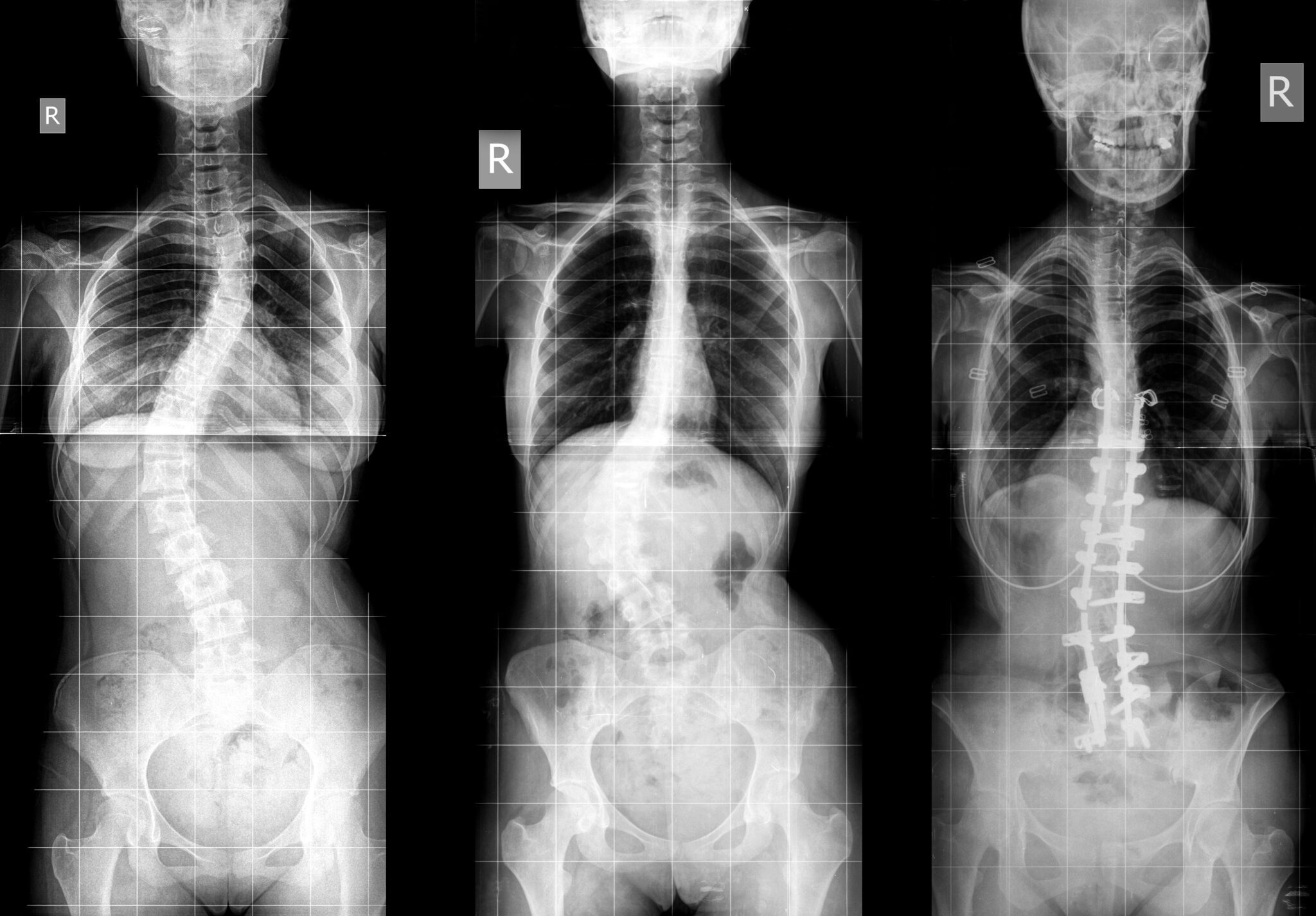
3. Imaging Studies
- X-rays:
- Standard Imaging: The primary diagnostic tool for scoliosis is an X-ray of the spine. This provides a clear image of the vertebrae and helps in assessing the degree of curvature.
- Cobb Angle Measurement: The severity of the scoliosis is determined by measuring the Cobb angle, which quantifies the degree of spinal curvature. A Cobb angle greater than 10 degrees is generally considered indicative of scoliosis.
- MRI or CT Scan:
- Further Evaluation: In some cases, especially if there is concern about an underlying condition (e.g., spinal cord abnormalities, tumors), an MRI or CT scan may be ordered for more detailed imaging.
4. Assessment of Growth and Maturity
- Risser Sign:
- An X-ray of the pelvis may be used to assess the Risser sign, which indicates the maturity of the skeletal system. This helps predict how much more a child may grow and the potential for scoliosis progression.
- Assessment of Pubertal Development:
- Evaluation of pubertal development can also provide information about growth potential and the likelihood of curve progression.
5. Additional Tests
- Pulmonary Function Tests:
- In cases of severe scoliosis, pulmonary function tests may be conducted to assess the impact of the curvature on lung function.
- Neurological Examination:
- A neurological exam may be performed to check for any neurological deficits that could be associated with the scoliosis or its underlying cause.
6. Differential Diagnosis
- Rule Out Other Conditions:
- The healthcare provider will consider other possible causes of spinal curvature or back pain, such as muscular conditions, infections, or congenital abnormalities.
Summary
The diagnosis of pediatric and adolescent scoliosis involves a thorough medical history, physical examination, and imaging studies, particularly X-rays, to assess the spinal curvature and its severity. The Cobb angle measurement is crucial in determining the degree of scoliosis. Additional tests, such as MRI, CT scans, pulmonary function tests, and neurological examinations, may be required depending on the individual case. Early detection and accurate diagnosis are essential for effective management and treatment planning.
What is the treatment for pediatric and adolescent scoliosis?
The treatment for pediatric and adolescent scoliosis depends on several factors, including the severity of the spinal curvature, the child’s age, the type of scoliosis, and the potential for further growth. The goals of treatment are to prevent the curve from worsening and to manage any symptoms. Here are the common treatment options:
1. Observation
- Mild Curvatures:
- Curves Less than 20 Degrees: For mild scoliosis (curves less than 20 degrees), especially in children who are still growing, the primary approach is observation. The child will have regular check-ups with a healthcare provider, including physical exams and X-rays, to monitor the curvature’s progression.
- Monitoring: The frequency of follow-up visits depends on the child’s age and growth rate.
2. Bracing
- Moderate Curvatures:
- Curves 20-40 Degrees: Bracing is often recommended for moderate scoliosis in children and adolescents who are still growing. The purpose of a brace is to prevent further progression of the curvature.
- Types of Braces:
- Thoracolumbosacral Orthosis (TLSO): The most common type, it is worn under clothing and can be custom-fitted.
- Milwaukee Brace: A full-torso brace with a neck ring, used less commonly today.
- Nighttime Bracing: Designed to be worn only while sleeping.
- Compliance:
- The effectiveness of bracing depends on wearing it as prescribed, usually for 16-23 hours a day. Compliance can be challenging, but it is crucial for preventing curve progression.
3. Physical Therapy and Exercise
- Supporting Muscles and Posture:
- Physical therapy may be recommended to strengthen core and back muscles, improve posture, and enhance overall physical function.
- Schroth Method:
- A specialized physical therapy approach focusing on scoliosis-specific exercises to elongate and de-rotate the spine.
4. Surgical Treatment
- Severe Curvatures:
- Curves Greater than 40-50 Degrees: Surgery may be recommended for severe scoliosis, particularly if the curve is progressive and causing symptoms or cosmetic concerns.
- Types of Surgery:
- Spinal Fusion: The most common surgical procedure, where vertebrae are fused together using bone grafts and metal rods, screws, or hooks to correct and stabilize the curve.
- Growing Rods: For younger children, growing rods can be surgically implanted and lengthened periodically as the child grows.
- Vertebral Body Tethering (VBT): A newer, less invasive procedure that uses a flexible cord to partially correct the curve and allow for continued growth.
- Postoperative Care:
- Recovery from scoliosis surgery can vary, with a typical hospital stay of several days and a gradual return to normal activities over months.
5. Alternative and Complementary Therapies
- Chiropractic Care, Yoga, Pilates:
- Some patients may seek alternative therapies. While these approaches can improve flexibility and comfort, they should not replace standard medical treatment.
6. Psychological Support
- Emotional and Social Aspects:
- Living with scoliosis, especially when wearing a brace or recovering from surgery, can affect a child’s self-esteem and social interactions. Support groups, counseling, and open communication with healthcare providers and family members are important.
7. Ongoing Monitoring
- Long-term Follow-up:
- Regular follow-up is essential to monitor curve progression, especially during growth spurts. Even after treatment, ongoing monitoring may be necessary to ensure the stability of the spinal curve.
Summary
The treatment approach for pediatric and adolescent scoliosis varies based on the curve’s severity, the child’s age, and the risk of progression. Observation is suitable for mild cases, while bracing is often used for moderate curves to prevent further worsening. In severe cases, surgery may be necessary to correct and stabilize the spine. Physical therapy and psychological support are important components of comprehensive care. The choice of treatment should be tailored to the individual needs of the patient and discussed thoroughly with healthcare providers.
Leave a Reply
You must be logged in to post a comment.