What are the symptoms of patellar tendonitis?
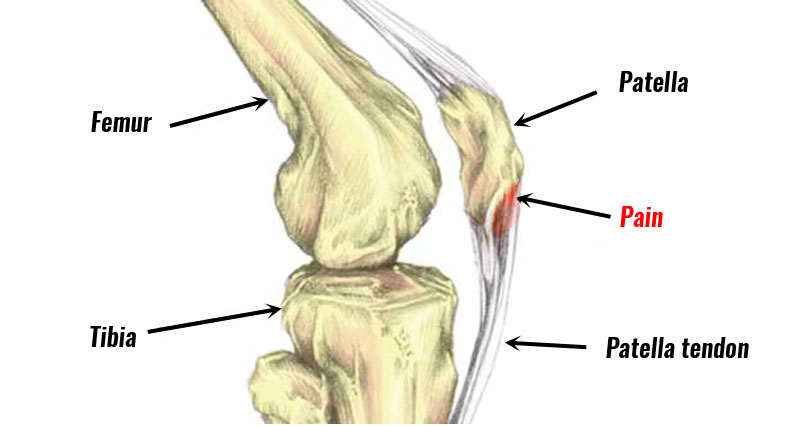
Patellar tendonitis, also known as jumper’s knee, is an overuse injury that affects the patellar tendon, which connects the kneecap (patella) to the shinbone (tibia). This condition is common among athletes who engage in jumping or repetitive knee movements. The symptoms can range from mild to severe depending on the extent of the injury.
Symptoms of Patellar Tendonitis:
- Pain below the kneecap: A key symptom is pain and tenderness just below the kneecap, where the patellar tendon attaches to the tibia. This pain may start as mild discomfort during or after physical activity.
- Pain that worsens with activity: The pain tends to increase with activities that put stress on the tendon, such as jumping, running, squatting, or climbing stairs. Over time, the pain can become more constant.
- Stiffness in the knee: Some people experience stiffness in the knee, particularly after periods of inactivity (such as in the morning or after sitting for a long time).
- Swelling or inflammation: There may be mild swelling around the knee, particularly below the kneecap, due to inflammation of the tendon.
- Weakness in the knee: The knee may feel weak or unstable, especially when trying to extend the leg or engage in physical activity.
- Pain with pressure: Applying pressure to the patellar tendon may cause tenderness or discomfort.
- Decreased range of motion: In severe cases, you may notice a reduced ability to bend or extend the knee.
Conclusion:
Patellar tendonitis typically develops gradually and can become more painful if left untreated. Rest, physical therapy, strengthening exercises, and sometimes anti-inflammatory treatments are commonly used to manage the condition.
What are the causes of patellar tendonitis?
Patellar tendonitis, or jumper’s knee, is primarily caused by repetitive stress and overuse of the knee joint. The following factors contribute to the development of patellar tendonitis:
1. Repetitive Strain
- High-Impact Activities: Repeated jumping, running, or activities that place high stress on the knee can lead to inflammation of the patellar tendon. Sports like basketball, volleyball, and soccer are common culprits.
- Overuse: Frequent, repetitive movements that stress the knee, especially without adequate rest, can cause strain on the tendon.
2. Biomechanical Issues
- Abnormal Patellar Tracking: Improper movement of the patella in its groove can place additional stress on the patellar tendon.
- Muscle Imbalances: Weakness or imbalance in the quadriceps, hamstrings, or calf muscles can affect knee mechanics and increase strain on the patellar tendon.
- Poor Foot Mechanics: Issues such as flat feet or improper footwear can contribute to abnormal knee mechanics and increased stress on the tendon.
3. Sudden Increases in Activity
- Rapid Change in Activity Level: Sudden increases in the intensity, duration, or frequency of physical activity can overload the patellar tendon, leading to inflammation.
4. Previous Injuries
- Past Injuries: A history of knee injuries or previous tendon issues can make the patellar tendon more susceptible to inflammation.
5. Age and Overuse
- Age-Related Changes: Tendons lose elasticity and strength with age, making them more prone to injury.
- Chronic Overuse: Long-term repetitive stress without adequate recovery can lead to chronic tendonitis.
6. Poor Technique or Training
- Improper Technique: Incorrect techniques in sports or exercise can place excessive stress on the knee and patellar tendon.
- Inadequate Warm-Up: Failing to properly warm up before physical activity can increase the risk of tendonitis.
7. Muscle Tightness
- Tight Muscles: Tightness in the quadriceps or hamstrings can increase the strain on the patellar tendon.
8. Training Errors
- Inappropriate Training Regimen: Engaging in training without proper conditioning, gradual progression, and adequate rest can contribute to the development of patellar tendonitis.
Addressing these causes through proper training, strengthening exercises, and modifying activities can help prevent and manage patellar tendonitis. If symptoms persist, it’s important to consult a healthcare professional for a comprehensive evaluation and appropriate treatment.
How is the diagnosis of patellar tendonitis made?
The diagnosis of patellar tendonitis involves a combination of a thorough medical history, physical examination, and sometimes imaging studies. Here’s how the diagnosis is typically made:
1. Medical History
- Symptom History: The healthcare provider will ask about the onset, duration, and nature of symptoms, including pain, tenderness, and any activities that may have contributed to the condition.
- Activity History: Information about recent or frequent physical activities, sports involvement, and any recent changes in activity levels is collected.
- Previous Injuries: Details about any past knee injuries or issues with the patellar tendon.
2. Physical Examination
- Inspection: The knee is examined for any visible signs of swelling or bruising.
- Palpation: Tenderness is assessed around the patellar tendon, particularly just below the kneecap where the tendon attaches to the tibia.
- Range of Motion: The healthcare provider will check for any limitations or pain during knee movement.
- Strength Testing: Assessment of the quadriceps and other muscles around the knee to identify any weakness or imbalances.
- Functional Tests: Tests may be performed to evaluate the knee’s response to activities that provoke symptoms, such as jumping or squatting.
3. Imaging Studies
- X-rays: While X-rays are not usually required to diagnose patellar tendonitis, they can be used to rule out other conditions such as fractures or bone abnormalities that may cause similar symptoms.
- Ultrasound: An ultrasound can help visualize inflammation of the patellar tendon and assess for any tears or structural changes.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of soft tissues and can help confirm the diagnosis by showing inflammation, tendon thickening, or any associated damage. It is often used if symptoms are persistent and do not improve with conservative treatment.
4. Differential Diagnosis
- Rule Out Other Conditions: The healthcare provider will differentiate patellar tendonitis from other conditions that cause similar symptoms, such as patellofemoral pain syndrome, bursitis, or meniscus tears.
5. Clinical Evaluation
- Clinical Tests: Specific clinical tests and maneuvers may be used to provoke symptoms and assess the function of the patellar tendon, such as the “patellar tendon palpation test” or “single-leg squat test.”
An accurate diagnosis is crucial for effective treatment. It helps to tailor a treatment plan that addresses the specific causes of the tendonitis and provides appropriate management strategies. If patellar tendonitis is diagnosed, a comprehensive treatment plan including rest, physical therapy, and possibly imaging-guided interventions can be developed to promote recovery and prevent recurrence.
What is the treatment for patellar tendonitis?
The treatment for patellar tendonitis aims to reduce pain, alleviate inflammation, and restore function to the knee. Treatment typically involves a combination of conservative measures, physical therapy, and, in some cases, more advanced interventions. Here’s a comprehensive approach to treating patellar tendonitis:
1. Rest and Activity Modification
- Rest: Avoid activities that exacerbate symptoms, such as jumping, running, or kneeling. Allow time for the tendon to heal.
- Activity Modification: Substitute high-impact activities with low-impact exercises like swimming or cycling to maintain fitness without stressing the knee.
2. Pain Management
- Medications: Over-the-counter pain relievers, such as acetaminophen or NSAIDs (e.g., ibuprofen, naproxen), can help reduce pain and inflammation.
- Ice Therapy: Applying ice packs to the knee for 15-20 minutes several times a day can help reduce swelling and pain.
- Heat Therapy: Applying heat may be helpful after the initial inflammation has decreased, especially if there is stiffness in the tendon.
3. Physical Therapy
- Strengthening Exercises: Focus on strengthening the quadriceps, hamstrings, and calf muscles to support the patellar tendon and improve knee stability. Exercises might include squats, leg presses, and straight leg raises.
- Flexibility Exercises: Stretching exercises for the quadriceps, hamstrings, and calf muscles can help reduce tension on the patellar tendon.
- Balance and Proprioception: Exercises to improve balance and proprioception (awareness of joint position) to help prevent further injury.
- Patellar Taping or Bracing: Techniques such as patellar taping or using a patellar tendon brace can provide additional support and improve patellar tracking.
4. Gradual Return to Activity
- Progressive Loading: Gradually reintroduce activities and increase intensity based on pain levels and improvement. Avoid jumping or running until the tendon has healed sufficiently.
- Warm-Up and Cool-Down: Properly warm up before activities and cool down afterward to prevent re-injury.
5. Advanced Interventions
- Extracorporeal Shock Wave Therapy (ESWT): This non-invasive treatment uses shock waves to promote healing in the tendon.
- Platelet-Rich Plasma (PRP) Therapy: Involves injecting a concentration of platelets from the patient’s own blood into the tendon to promote healing and reduce inflammation.
- Ultrasound-Guided Injections: Corticosteroid or hyaluronic acid injections may be used to reduce inflammation and provide temporary relief.
6. Surgical Treatment
- Surgery: If conservative treatments fail and symptoms persist, surgery may be considered. Procedures may include:
- Tendon Debridement: Removal of damaged tissue from the patellar tendon.
- Tendon Repair: Repair of any tears or significant damage to the tendon.
- Surgical Realignment: Correction of any alignment issues contributing to the problem.
7. Preventive Measures
- Proper Technique: Ensure correct technique in sports and exercises to prevent future injuries.
- Strengthening and Conditioning: Maintain a regular exercise routine focusing on muscle balance and flexibility.
- Footwear: Use appropriate footwear to support knee alignment and reduce stress on the patellar tendon.
The treatment plan for patellar tendonitis is individualized based on the severity of the condition, the patient’s activity level, and response to initial treatments. A healthcare provider or physical therapist can help design a specific plan to address the symptoms and underlying causes effectively.
Leave a Reply
You must be logged in to post a comment.