What are the symptoms of patellar dislocations?
The symptoms of patellar dislocation can vary in severity and may include:
- Sudden Pain: Intense pain in the knee, often felt immediately after the dislocation occurs.
- Visible Deformity: The kneecap may appear out of its normal position, often shifted to the outside of the knee (lateral dislocation).
- Swelling: Rapid swelling around the knee joint due to fluid accumulation and inflammation.
- Limited Range of Motion: Difficulty bending or straightening the knee fully.
- Instability: A feeling of instability or “giving way” in the knee, especially when attempting to walk or put weight on the leg.
- Bruising: Discoloration around the knee due to bleeding from damaged blood vessels.
- Tenderness: The area around the kneecap may be sensitive to touch.
- Popping or Clicking Sensation: Some individuals may report a popping or clicking sound at the time of dislocation.
These symptoms typically prompt individuals to seek medical attention, as a dislocated patella often requires prompt evaluation and treatment to prevent further damage and to stabilize the knee joint.
What are the causes of patellar dislocations?
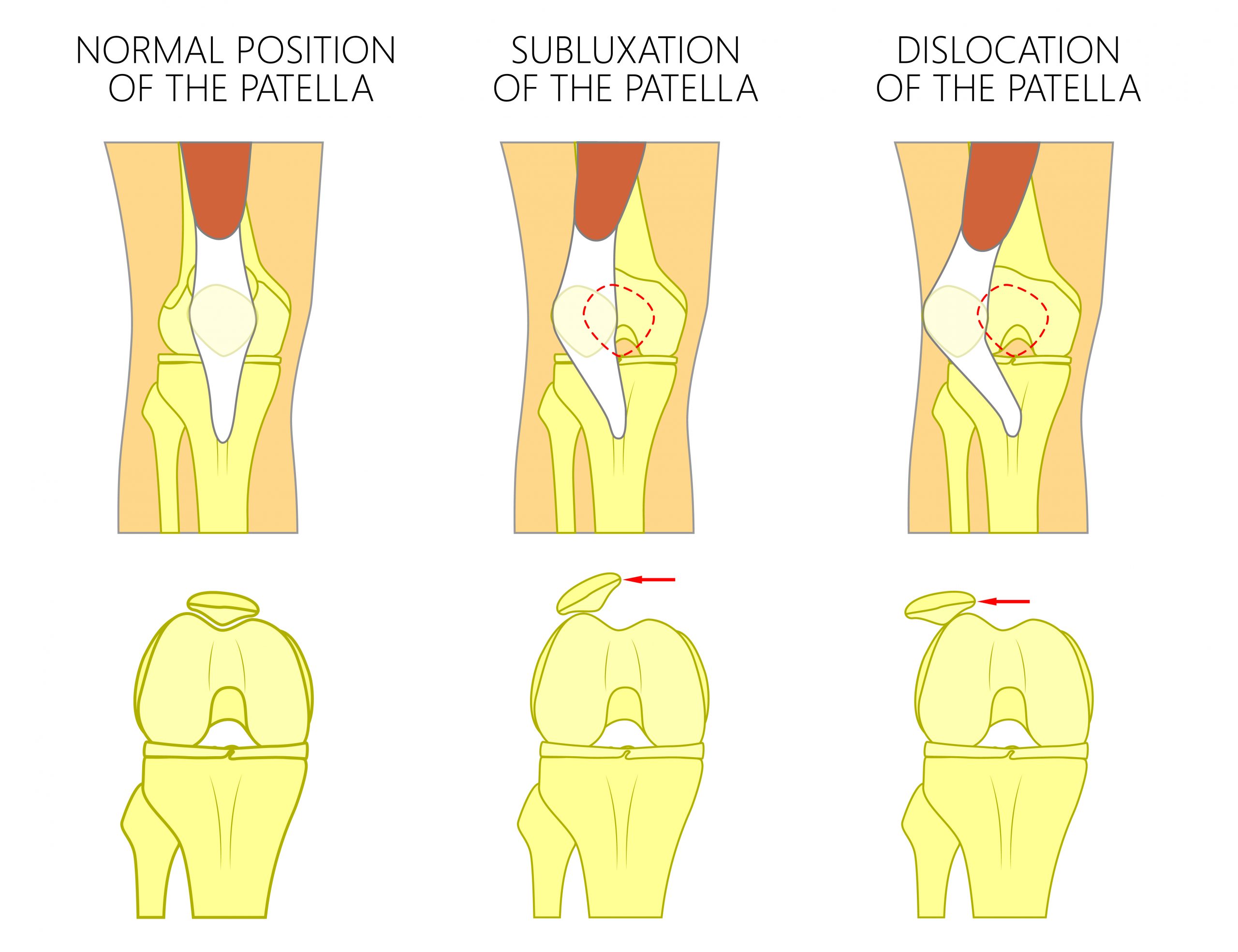
Patellar dislocations occur when the kneecap (patella) slips out of its normal position in the groove at the end of the thigh bone (femur). The causes of patellar dislocations can vary and include:
- Trauma or Injury:
- Direct impact to the knee, such as during sports or accidents.
- Sudden twisting movements, which can occur during activities like running or jumping.
- Weak or Imbalanced Muscles:
- Weakness in the quadriceps, particularly the vastus medialis obliquus (VMO), can lead to poor patellar tracking.
- Imbalances between the inner and outer quadriceps muscles can cause the patella to shift laterally.
- Abnormal Anatomy:
- Structural abnormalities, such as a shallow trochlear groove (the groove where the patella sits), can predispose individuals to dislocations.
- Patella alta (high-riding patella) or patella baja (low-riding patella) can also increase the risk.
- Ligament Laxity:
- Conditions that cause hypermobility or increased laxity in the ligaments can make it easier for the patella to dislocate.
- Connective tissue disorders, such as Ehlers-Danlos syndrome, can contribute to this.
- Previous Dislocations:
- A history of previous dislocations can increase the likelihood of future occurrences, as the ligaments and soft tissues may become stretched or weakened.
- Poor Biomechanics:
- Abnormalities in gait or alignment, such as flat feet or excessive foot pronation, can alter the forces acting on the knee and increase the risk of dislocation.
- High-Impact Sports:
- Athletes participating in high-impact sports (e.g., football, basketball, soccer) are at a greater risk due to the nature of the movements involved.
Conclusion:
Patellar dislocations can result from a combination of traumatic injuries, muscle imbalances, anatomical variations, and previous dislocations. Understanding these causes can help in preventing future incidents and guiding treatment strategies.
How is the diagnosis of a patellar dislocation made?
The diagnosis of a patellar dislocation is typically made through a combination of the following methods:
- Medical History:
- The doctor will begin by asking about the patient’s symptoms, including the nature of the injury, the onset of pain, any previous dislocations, and how the injury occurred.
- Physical Examination:
- The physician will examine the knee for signs of dislocation, including visible deformity (the patella may be displaced), swelling, tenderness, and bruising.
- The range of motion will be assessed to determine any limitations or instability in the knee.
- Palpation:
- The doctor may palpate the knee to locate the position of the patella and assess any accompanying injuries to surrounding structures, such as ligaments and tendons.
- Imaging Studies:
- X-rays: X-rays are often the first imaging test performed to confirm the dislocation and rule out any associated fractures in the knee or surrounding bones.
- MRI: In some cases, an MRI may be ordered to evaluate soft tissue structures, including ligaments, cartilage, and muscles. This can help assess any damage to the ligaments or other tissues that may have occurred during the dislocation.
- Special Tests:
- The doctor may perform specific physical tests to assess the stability of the knee and patella. This may include tests for patellar apprehension, which checks for any discomfort or fear of dislocation when the patella is pushed laterally.
Conclusion
A thorough clinical assessment, combined with imaging studies, is essential in diagnosing patellar dislocation and evaluating any associated injuries. Prompt diagnosis is crucial for effective treatment and rehabilitation.
What is the treatment for a patellar dislocation?
The treatment for a patellar dislocation aims to reduce pain, restore normal knee function, and prevent future dislocations. The approach can vary based on the severity of the dislocation, the presence of associated injuries, and the patient’s overall health. Here’s a detailed overview of the treatment options:
Immediate Treatment
- Reduction:
- If the patella is dislocated, the first step is to realign it into its proper position. This process, called reduction, is usually performed in a clinical setting. A healthcare professional will gently manipulate the kneecap back into place.
- Immobilization:
- After reduction, the knee may be immobilized using a brace or splint to prevent movement and allow the ligaments and tissues to heal. This immobilization typically lasts for a few weeks, depending on the injury’s severity.
Conservative Treatment
- Rest:
- Limiting physical activity and avoiding weight-bearing on the affected leg is crucial during the initial healing phase.
- Ice Therapy:
- Applying ice packs to the knee can help reduce swelling and pain. Ice should be applied for 15-20 minutes every few hours during the first few days after the injury.
- Elevation:
- Keeping the leg elevated can also help minimize swelling.
- Compression:
- Using an elastic bandage or compression wrap can provide support and reduce swelling.
- Pain Management:
- Over-the-counter pain relievers such as ibuprofen or acetaminophen can be used to alleviate pain and reduce inflammation.
Rehabilitation
- Physical Therapy:
- Once the acute pain and swelling have decreased, physical therapy is often recommended to restore strength, flexibility, and stability in the knee. A physical therapist will design a tailored exercise program that may include:
- Range of motion exercises to improve flexibility.
- Strengthening exercises for the quadriceps, hamstrings, and hip muscles.
- Balance and proprioception exercises to enhance joint stability.
- Gradual Return to Activity:
- As strength and stability improve, individuals can gradually return to their normal activities and sports, guided by their healthcare provider or physical therapist.
Surgical Treatment
In cases where conservative treatment fails or if there are recurrent dislocations, surgical options may be considered:
- Lateral Release:
- This procedure involves cutting the tight lateral retinaculum (the tissue on the outside of the kneecap) to allow for better tracking of the patella.
- Medial Patellofemoral Ligament (MPFL) Reconstruction:
- If the ligament that helps stabilize the patella is torn or damaged, it may be reconstructed using a graft.
- Realignment Procedures:
- In some cases, the alignment of the patella or the bones of the knee may need to be surgically corrected to prevent future dislocations.
- Arthroscopy:
- If there are associated cartilage injuries or loose bodies in the knee joint, arthroscopic surgery may be performed to clean up the joint.
Post-Treatment Care
- Follow-Up:
- Regular follow-up appointments are important to monitor healing and ensure the proper progression of rehabilitation.
- Long-Term Management:
- Individuals with a history of patellar dislocation may benefit from ongoing strength training and stability exercises to reduce the risk of future dislocations.
Conclusion
Treatment for patellar dislocation varies depending on the severity and individual circumstances. Early intervention and a structured rehabilitation program are crucial for optimal recovery and prevention of recurrence. Consulting with healthcare professionals for a personalized treatment plan is essential.
Leave a Reply
You must be logged in to post a comment.