What are the symptoms of osteopenia?
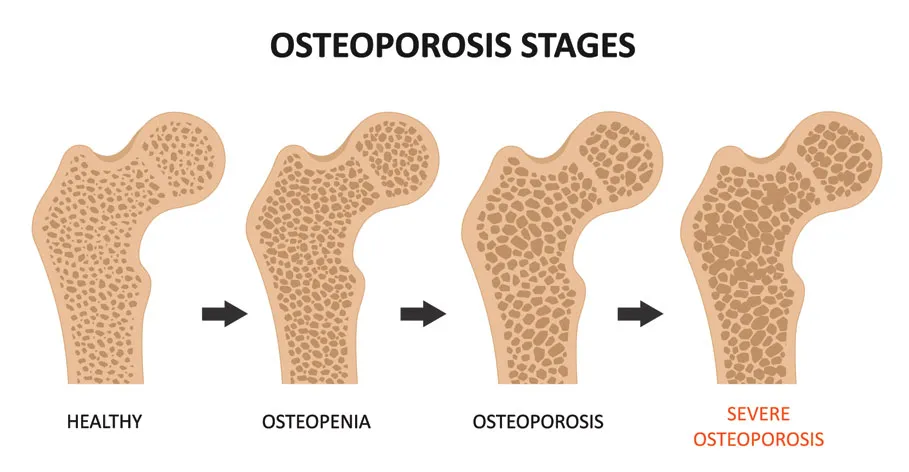
Osteopenia is a condition characterized by lower-than-normal bone density, which can increase the risk of developing osteoporosis and bone fractures. It is often considered a precursor to osteoporosis. One of the challenges with osteopenia is that it often does not present with obvious symptoms in its early stages. However, as the condition progresses, individuals may begin to experience some signs. Here are the key points regarding the symptoms:
Symptoms of Osteopenia
- No Symptoms in Early Stages:
- Many individuals with osteopenia do not experience any noticeable symptoms, making it challenging to detect without a bone density test (DEXA scan).
- Signs and Symptoms as Condition Progresses:
- Bone Fractures: Increased susceptibility to fractures, particularly in weight-bearing bones (such as the spine, hips, and wrists), may occur. These fractures can happen with minimal trauma or in some cases, with no apparent cause.
- Back Pain: Pain may develop in the back due to fractures in the vertebrae or degenerative changes in the spine. A compression fracture of the vertebrae can lead to significant pain and a stooped posture.
- Loss of Height: A gradual decrease in height can occur over time due to vertebral compression fractures or other changes in the spine.
- Stooped Posture (Kyphosis): A hunched or stooped posture may develop, often due to spinal fractures or weakening bones.
- Increased Risk of Falls: The weakened and more fragile bones can lead to an increased risk of falls, which are often further complicated by a reduced ability to recover from injuries.
Diagnosis:
Since osteopenia typically does not produce any symptoms until significant bone loss has occurred, it is essential to have regular bone density screenings, particularly for individuals at higher risk (such as postmenopausal women, older adults, and those with a family history of osteoporosis). These screenings can help identify low bone density early, even in the absence of symptoms.
Conclusion:
If you are concerned about your bone health or risk factors for osteopenia or osteoporosis, it’s important to discuss these with a healthcare professional. They can recommend appropriate screenings, preventive measures, and potential treatment options to help maintain bone density and overall skeletal health.
What are the causes of osteopenia?
Osteopenia is a condition characterized by lower-than-normal bone density, which can increase the risk of developing osteoporosis and bone fractures. The causes of osteopenia are multi-faceted and can be attributed to various factors, including lifestyle choices, medical conditions, medications, and genetic predispositions. Here are some of the main causes:
1. Age:
- As people age, bone density tends to decrease naturally due to a decrease in bone formation and an increase in bone resorption, especially after menopause in women.
2. Hormonal Changes:
- Estrogen Deficiency: In women, menopause leads to a drop in estrogen levels, which plays a critical role in maintaining bone density. This change is a significant risk factor for both osteopenia and osteoporosis.
- Testosterone Deficiency: In men, low testosterone levels can also lead to decreased bone density.
3. Dietary Factors:
- Low Calcium Intake: Inadequate calcium intake over time can hinder bone development and maintenance.
- Vitamin D Deficiency: Vitamin D is essential for calcium absorption in the body; insufficient levels can lead to decreased bone density.
- Poor Nutrition: A diet lacking in essential nutrients (e.g., protein, magnesium) can adversely affect bone health.
4. Lifestyle Factors:
- Sedentary Lifestyle: Lack of weight-bearing exercise can weaken bones; physical activity is essential for maintaining or improving bone density.
- Smoking: Tobacco use has been linked to reduced bone density and an increased risk of fractures.
- Excessive Alcohol Consumption: Heavy drinking can interfere with calcium balance and bone formation.
5. Medical Conditions:
- Endocrine Disorders: Conditions such as hyperthyroidism (overactive thyroid), hyperparathyroidism, and adrenal diseases can affect bone density.
- Malabsorption Disorders: Conditions like celiac disease, Crohn’s disease, and ulcerative colitis can impede the absorption of vital nutrients.
- Chronic Kidney Disease: This can lead to imbalances in calcium and phosphate, affecting bone health.
- Anorexia Nervosa: Eating disorders can lead to inadequate nutrition and hormone imbalances that negatively impact bone density.
6. Medications:
- Corticosteroids: Long-term use of corticosteroids can inhibit bone formation and increase bone resorption, leading to a decrease in bone density.
- Certain Anticonvulsants: Some medications used to treat seizures can also adversely affect bone density.
- Other Medications: Medications such as proton pump inhibitors (for acid reflux) may interfere with calcium absorption.
7. Genetics:
- Family history of osteoporosis or low bone density can increase an individual’s risk of developing osteopenia.
8. Other Factors:
- Gender: Women are generally at a higher risk for developing osteopenia and osteoporosis than men.
- Body Frame Size: Individuals with smaller body frames tend to have less bone mass and may be at greater risk.
Conclusion:
It’s important for individuals, especially those at higher risk, to be aware of these causes and seek guidance from healthcare professionals. Early detection through bone density screening and addressing risk factors through lifestyle changes, dietary adjustments, and managing medical conditions can help mitigate the risk of developing osteopenia and osteoporosis.
How is the diagnosis of osteopenia made?
The diagnosis of osteopenia is primarily made through a combination of risk assessment and imaging studies, particularly through a bone density test called a dual-energy X-ray absorptiometry (DEXA or DXA) scan. Here are the steps typically involved in diagnosing osteopenia:
1. Medical History:
- Risk Factor Assessment: The healthcare provider will take a comprehensive medical history, including family history of osteoporosis, personal history of fractures, any medical conditions that could affect bone health, and lifestyle factors such as diet, activity levels, smoking, and alcohol consumption.
- Medication Review: Discussion of any medications currently being taken that might affect bone density, such as corticosteroids or anticonvulsants.
2. Physical Examination:
- A physical exam may be conducted to assess general health and identify any potential signs of bone loss or related conditions.
3. Bone Density Test (DXA Scan):
- DEXA Scan: This is the most common and effective method for diagnosing osteopenia. The DEXA scan measures bone mineral density (BMD) at key sites like the hip and lumbar spine.
- T-Score: The results of the DEXA scan are compared to the bone density of a healthy young adult of the same sex. The score that results from this comparison is called the T-score.
- A T-score of:
- Above -1.0: Normal bone density
- Between -1.0 and -2.5: Osteopenia (low bone density)
- Below -2.5: Osteoporosis
4. Additional Imaging Studies (if necessary):
- In some cases, other imaging tests, such as X-rays or CT scans, may be used to identify fractures, assess bone structure, or look for changes in the spine.
5. Lab Tests:
- Blood tests may be performed to evaluate calcium, vitamin D, thyroid function, and other factors that influence bone health. These tests can help rule out other conditions that may be contributing to low bone density.
Conclusion:
If you are at risk for osteopenia or osteoporosis, it is important to discuss your concerns with a healthcare provider. Regular screening and appropriate interventions can help manage bone health effectively. Early detection increases the opportunity to implement lifestyle changes and potentially medication to protect against further bone loss.
What is the treatment for osteopenia?
The treatment for osteopenia focuses on improving bone density and reducing the risk of progression to osteoporosis. The approach typically involves lifestyle modifications, dietary changes, and, in some cases, medications. Here are the common components of treatment for osteopenia:
1. Lifestyle Modifications:
- Weight-Bearing Exercise: Engage in regular physical activity that includes weight-bearing and muscle-strengthening exercises. Activities such as walking, jogging, dancing, and resistance training can help strengthen bones.
- Balance Training: Incorporating balance and coordination exercises can help prevent falls, which are a risk for individuals with low bone density.
2. Dietary Changes:
- Calcium-Rich Foods: Increase intake of calcium through diet. Good sources include dairy products (milk, yogurt, cheese), leafy green vegetables (kale, broccoli), fortified foods (cereals, plant-based milk), and fish with bones (sardines, salmon).
- Vitamin D: Ensure adequate vitamin D intake to support calcium absorption. You can get vitamin D through sunlight exposure, foods like fatty fish, fortified products, and supplements if necessary.
- Balanced Diet: Consume a well-rounded diet that includes sufficient protein, fruits, and vegetables to support overall health and bone density.
3. Lifestyle Changes:
- Quit Smoking: Smoking is detrimental to bone health; quitting can positively impact bone density.
- Limit Alcohol Intake: Excessive alcohol can lead to bone loss. It’s advisable to limit consumption to no more than one drink per day for women and two drinks per day for men.
4. Medications:
- Biphosphonates: These are commonly prescribed for individuals at high risk of fracture or those with more advanced bone loss. They help to slow down bone resorption and may help improve bone density.
- Selective Estrogen Receptor Modulators (SERMs): These may be used, especially in postmenopausal women, to help maintain bone density and reduce the risk of fractures.
- Hormone Replacement Therapy (HRT): In some cases, hormone therapy may be considered for postmenopausal women to help maintain bone density, but it also comes with potential risks and benefits that should be discussed with a doctor.
- Denosumab: An injectable medication that can reduce bone resorption and is used in certain cases.
5. Regular Monitoring:
- Regular follow-up with healthcare providers is essential for monitoring bone density, assessing treatment effectiveness, and making necessary adjustments to the treatment plan.
6. Supplementation:
- Calcium and vitamin D supplements may be recommended for individuals who cannot meet their needs through diet alone. The exact dosage should be tailored to individual requirements and discussed with a healthcare provider.
Conclusion:
Management of osteopenia is a proactive approach aimed at enhancing bone health and preventing further bone loss. Individuals diagnosed with osteopenia should work closely with healthcare professionals to develop a personalized plan that includes lifestyle modifications, dietary changes, and, if necessary, medications. Regular check-ups and adjustments to the treatment plan based on bone density assessments are crucial for maintaining optimal bone health.
Leave a Reply
You must be logged in to post a comment.